Shanmuganathan Rajasekaran, Siddharth Aiyer, and Rishi Mugesh Kanna
INTRODUCTION
Management options in spondylolisthesis vary with the etiology, morphology, grade of slip and severity of dysplasia at the affected segment. While the treatment options are well defined in most situations, the optimal management of high grade spondylo listhesis has generated significant controversy.1-4 Most authors agree that symptomatic high grade spondylolisthesis in pediatric and adolescent population is an indication for surgical fusion. The point of debate is whether a reduction of the spondylolisthesis should be performed along with the fusion procedure or an in-situ fusion is a satisfactory strategy in such a clinical scenario.2-10 In-situ fusion procedures have been associated with reports of slip progression, higher risk of pseudoarthrosis and persistence of cosmetic deformity.5,11-13 Proponents of reduction cite the advantages of improved biomechanics, higher fusion rates and cosmetic correction of deformity.6-9 However, reduction of high grade slips has been associated with significant risk of complications including neurological deficit.9,14-16 Adding to this existing debate, there are reports published, which have documented comparable clinical outcome between in-situ fusion and reduction and fusion at long term follow up.17-19
Grading of Spondylolisthesis
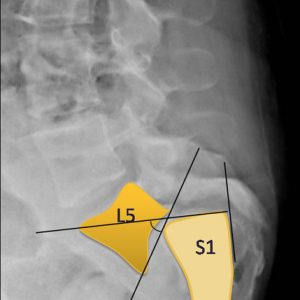
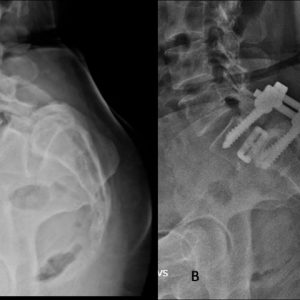
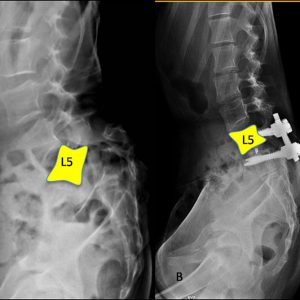
As per Meyerding’s grading, high grade spondylolisthesis has been defined as slips which have translation of more than 50% at the spondylolisthetic segment and this includes grade III (50-75%), grade IV (more than 75%) and grade V where the vertebral body has completely slipped anterior to the caudal segment and is termed as spondyloptosis (Fig. 4-1).
De Wald proposed a modified radiological assessment index for quantifying the severity of slip. The sacral (S1) superior end plate and anterior surface of the S1 are divided into 10 segments. The slip is expressed as two numerical values to signify the location of the posterior inferior corner along the superior S1 end plate and the location of the anterior inferior corner of L5 along the anterior surface of S1. This radiological parameter thus not only considers the anterior translation but also includes an assessment of the slip angle.
Classification for Spondylolisthesis
Numerous classification systems have been proposed for spondylolisthesis based on the morphological and etiological features. These include the Wiltse, Newman and McNab classification which allows to clearly communicate the etiology for the spondylolisthesis.20 The Marchetti and Bartolozzi classification offers prognostic value for slip progression under the high and low dysplastic subcategorization of developmental slips.21
The concept of high grade spondylolisthesis has been incorporated into the clinical management and decision making process by the Spine Deformity Study Group (SDSG).22 The SDSG classification takes into account the regional spinopelvic balance and global spinal balance in the high grade spondylolisthesis and offers guidelines to assess the need for reduction of the slip.23,24
Factors Associated with Progression
The risk factors for progression include age at presentation, slip angle, developmental slips associated with dysplasia of posterior elements and higher grade of slip. High dysplastic spondylolisthesisis characterized by major developmental abnormality of the lumbo-sacral junction. They may include formation defects of the L5 posterior elements, trapezoidal L5 vertebral body and doming of the upper end plate of the sacrum. High dysplastic slips are prone to develop progression especially in the pediatric and adolescent age groups due to significant remaining growth potential. The slip angle defined by the angle formed between the inferior end plate of the L5 and the perpendicular drawn to the line drawn along the posterior border of the sacrum and the lumbosacral kyphosis also affects the chance of progression (Fig. 4-2). More than the percentage of translation between the L5-S1 segments, a higher slip angle and more pronounced lumbosacral kyphosis contributes to progression.
With progressive increase in the slip angle and lumbosacral junction kyphosis, the L5 vertebra assumes a more vertical orientation. Compensatory lumbar lordosis increases at the cephalic segments and the sacrum and pelvis become more retroverted. These factors turn the weight bearing forces into shear forces at the lumbosacral junction resulting in propagation of the slip.
Spino-pelvic Parameters in High Grade Spondylolisthesis
High grade spondylolisthesis affects the overall sagittal balance of the individual and creates a significant biomechanical imbalance. Various compensatory mechanisms develop as a result of this imbalance. The severe lumbosacral kyphosis leads to a compensatory increase in lumbar lordosis at the cephalic segments. The normal anatomical position of the pelvis is that of anteversion; however, in unbalanced high grade slips the pelvis assumes a retroverted position. The pelvic retroversion in turn produces an over active hamstring spasm as a compensatory mechanism. This hamstring spasm gives rise to the typical crouched gait seen with high grade slips; such that the hips and knees assume an attitude of flexion.
There is an abnormal sacro-pelvic anatomy and compensatory mechanism affects the sacro-pelvic orientation assumed on upright position and during ambulation. High grade slips are frequently associated with a positive sagittal balance. The altered position and compensatory mechanisms compromise the biomechanical expenditure on assuming upright position and result in the clinical symptoms.
The pelvic incidence (PI) is an anatomical parameter that is constant after adolescence and is defined as the angle subtended between a perpendicular at the midpoint of the upper end of the sacrum and a line drawn from the femoral head to the midpoint of the upper end of the sacrum. Higher PI is seen in spondylolisthesis when compared to normal population and a linear increase has been noted with higher grade of spondylolisthesis.
The sacral slope is the angle subtended by the upper end plate of the sacrum to the horizontal plane. The pelvic tilt is the angle subtended between the line joining the mid-point of the upper end plate of sacrum to the femoral head and a vertical line drawn at the femoral heads. The PI is considered to be the sum of the sacral slope and pelvic tilt. Though PI does not change (anatomical constant) after adolescence, the changes in sacral slope and pelvic tilt determine the eventual sacro-pelvic orientation.
Sacro-pelvic balance
The SDSG group has proposed the sacro-pelvic balance and orientation, as determined by the sacral slope and pelvic tilt.22 In cases with high PI where the sacral slope is high and pelvic tilt is low, the sacro-pelvic orientation is closer to normal and is considered as a balanced sacro-pelvic orientation. In cases with higher pelvic tilt and lower sacral slope, the pelvis is retroverted and the pelvis is considered an unbalanced orientation.
Spino-pelvic balance
The spino-pelvic balance is based on the assessment of the C7 plumb line. Normally, this line passes close to the posterior superior corner of S1. The sagittal profile of each region—cervical, thoracic and lumbar—affects the adjacent segment and contributes to the overall global spinal balance. In high-grade spondylolisthesis, the abnormal anatomy and orientation results in an increase in the lumbar lordosis as a compensation for the retroverted pelvis, and this can affect global spino-pelvic balance causing a sagittal imbalance.
CLINICAL FEATURES
Patients with high-grade spondylolisthesis present with a diverse set of clinical symptoms. Back pain is the most common presentation and results from the instability caused by the vertebral slip. They often have a cosmetic deformity resulting from the kyphosis at the lumbosacral junction, and this is frequently associated with pediatric and adolescent high-grade slips. High grade slip compromises the spinal canal and neural foramen diameters, and, hence, patients often present with radiculopathy of the exiting nerve root, most commonly the L5 root. Patients also present with neurogenic claudication, motor weakness and occasionally bowel bladder incontinence arising out of cauda equina compromise. Features of neurological dysfunction are seen more often in adults; while in pediatric and adolescent slips, neurological deficit is an uncommon presenting feature. High grade slips at L5-S1 junction need to have a meticulous neurological examination as frequently they may present with subtle features of neurological dysfunction as evidenced by a decreased anal sphincter tone and voluntary contraction of the anal sphincter. Minimal motor weakness in the extensor hallucius longus due to compromise of the L5 exiting nerve root may be overlooked and, hence, needs careful attention.
Physical signs include a palpable step-off over the midline with a prominence of the sacrum and flattening of the buttocks. The kyphosis at the L5-S1 junction is compensated with an exaggerated lumbar lordosis at the cephalic segments which is well appreciated on clinical examination. The hamstrings are tight in response to the slip and as a compensatory mechanism, lead to retroversion of the pelvis. These compensatory mechanisms result in a forward stooped posture with flexion at the knee and hips. The lumbosacral kyphosis, exaggerated lumbar lordosis, retroverted pelvis and flexed position of the hips and knees result in a typical posture and a crouched gait on ambulation.
INVESTIGATIONS
High grade spondylolisthesis needs to be evaluated with whole spine standing radiographs in antero-posterior and lateral projections. The percentage of translation and lumbosacral kyphosis is a dynamic entity. Radiographic evaluation in a supine position would underestimate the severity of slip and, therefore, standing radiographs are preferred. Whole spine radiographs are needed to evaluate the spino-pelvic parameters of pelvic incidence, pelvic tilt, sacral slope and the global spinal sagittal balance. Dynamic films of the lumbosacral spine in flexion and extension are required to assess the instability at the involved segment.
The Ferguson view is a specialized view to best assess the lumbosacral junction. The size of the transverse process of the L5 and the morphology of the sacral ala must be assessed if a posterolateral fusion is being contemplated. The anteroposterior radiographs in high grade slips have a typical appearance of an Inverted Napoleon Hatcaused by the body of the L5 lying anterior to the sacrum. Oblique radiographs help visualize the region of the pars interarticularis and may be performed to document the presence of a spondylolysis.
The anteroposterior radiographs are assessed for any evidence of dysplasia of the posterior elements. High grade slip may be associated with a spina bifida occulta, and this should be noted to avoid inadvertent injury to the dural sac and neural tissues during the surgical exposure. The radiographs should be evaluated for other evidence to suggest high dysplastic slip such as trapezoidal L5 vertebral body, doming of the sacrum and elongated pars interarticularis. The percentage of translation is assessed on the lateral radiograph to document the grade of slip as per Meyerding’s classification. The lumbosacral kyphosis is assessed using the slip angle or lumbosacral angle of Dubousset’s on the lateral radiograph.
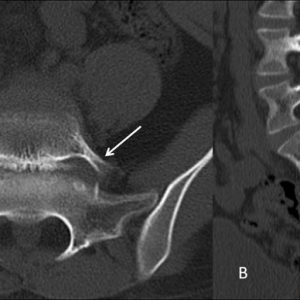
High grade slip may need evaluation with a CT scan to assess the dimensions of the L5 pedicle on the axial sections, because frequently these may be significantly dysplastic, precluding a safe screw insertion (Fig. 4-3). The CT scan can also confirm the presence of spondylolysis or a “break in the pars” when the visualization is inadequate on the radiographs.
MRI is required to assess the severity of compromise of central canal, lateral recess and neural foramen of the lumbar spine. There is considerable stress at the adjacent levels in such high-grade slips, which can lead to early disc degeneration at the adjacent levels. MRI also helps to evaluate the status of the adjacent level disc and helps in the decision of ultimate superior extent of fusion. The T2 weighted MRI images on the sagittal section may show signal changes in the region of the pars in acute slips. The compression of the exiting nerve roots is clearly seen in the axial sections which show the offending fibrocartilage tissue at the region of the pars defect.
MANAGEMENT STRATEGIES
Management strategies for high grade spondylolisthesis have been controversial. This stems from the fact, that studies documenting natural course of the disease are few, and, in most series, they are confounded by the heterogenicity of the study population. This is due to a diverse etiology of spondylolisthesis being included in the same cohort. High grade spondylolisthesis is frequently developmental in origin and occasionally arise in lytic spondylolisthesis. Degenerative spondylolisthesis is rarely associated with high grade slips.
Observation
In a long term follow up study of grade III and IV slips over 18 years of age, the authors noted that up to 36% of the patients treated non-surgically were asymptomatic. Even when patients presented with neurological symptoms, 45% were mild in nature, and rarely overt neurological deficit was reported.7 The behavior of high grade slips is dependent on the growth potential and thus adult and pediatric high grade slips need to be evaluated separately. While asymptomatic adult high grade slips can be observed, the same is not true in pediatric population. Pediatric slips are liable to progress and, hence, will need surgical stabilization to prevent slip progression.
Surgical treatment
The controversies in the surgical management of high grade slips have been raised with regards to levels of fusion, need for reduction, need for decompression, the nature of instrumentation, surgical approaches and fusion strategy. The surgical option in treatment of high grade spondylolisthesis includes 3 basic options—in-situ fusion, partial reduction and fusion, and complete reduction. Each of these procedures may be combined with a posterior decompression based on the clinical neurological status and presenting symptoms. There are additional modifications in surgical approach, with some authors favoring an anterior L5-S1 fusion procedure in addition to posterior instrumentation and fusion. In the clinical scenario of spondyloptosis, a complete L5 vertebral resection has been described by authors to reduce L4 on to the sacrum.25,26
Preoperative planning
The preoperative planning includes assessment of reducibility of the slip using dynamic films in flexion and extension. Frequently in high grade dysplastic slips, the pedicles of L5 are narrow and may not accommodate even smaller diameter pedicle screws. The L5 pedicle may need CT evaluation and posterior spine exposure must be done with care as accompanying posterior element defects may increase the risk of dural sac injuries. Claudio et al. have developed a parameter of severity index to identify low-dysplastic and high dysplastic developmental slips.27 The severity index forms a guideline to decide on the need for reduction of slip. A severity index >20 % is considered to be an indication to reduce the spondylolisthesis. The authors have also proposed the concept of stable zone to help guide scenarios when the fusion should be extended to L4 or higher.27
The preoperative planning for surgical process of reduction of high grade slips includes the use of neuro-monitoring. Pedicle screws may be stimulated to check for changes in the electromyographic monitor, which may suggest pedicle screw breach.28 Nerve root stimulation for the lumbar roots is routinely used to assess the adequacy of decompression and to identify any developing neurological deficit during the process of reduction. The normal threshold noted in lumbar nerve roots stands at 2mA. In high grade spondylolisthesis, this may rise higher and returns towards baseline following adequate decompression.
In-situ fusion
In-situ fusion is performed with or without decompression in patients presenting without neurological deficit. A posterior or posterolateral fusion may be performed, and retaining the posterior elements helps to increase the area available for the fusion bed. In-situ fusions can be combined with trans-vertebral sacral fixation using screws or fibular strut graft which provides additional anterior column support. This may reduce the chance of progression of slip and pseudoarthrosis. The advantages of in-situ fusion include lower risk of neurological deficit, shorter operative times and blood loss. However, there are reports of patients developing cauda equina even with in-situ fusion. The reports suggested that the muscle relaxation at the time of general anesthesia may have compromised the neural canal further resulting in a cauda equina syndrome.
In-situ posterolateral fusion places the fusion mass at risk of shear forces as the transverse process of the L5 vertebra lies anterior to the sacral ala. Small area of the transverse process can increase the risk of pseudoarthrosis.3 However, in comparison to posterolateral fusion procedures, circumferential fusion procedures have documented lower pseudoarthrosis rates.1,3,11 Interestingly, various authors have reported that in spite of higher pseudoarthrosis with in-situ fusion procedures, the clinical and functional outcomes of in-situ fusion are comparable to circumferential fusion procedure with reduction of the spondylolisthetic slip.4 Reduction and circumferential fusion procedures are associated with increased operative times, blood loss and higher complication rates.19 Poussa et al. reported on the long term comparative outcomes for in-situ fusion versus reduction and fusion. The authors reported no significant difference for the clinical and functional outcomes between the two strategies.18
From the authors’ perspective, in-situ fusion may be considered in high grade spondylolisthesis when it is associated with balanced pelvis (low pelvic tilt), sagittally balanced spine, and large transverse process of L5, without significant radicular symptoms or neurological symptoms.
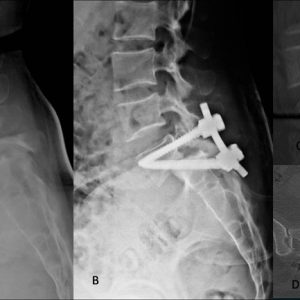
When the lumbosacral kyphosis is reducible, intraoperative positioning of the hip in extension can reduce the lumbosacral kyphosis. The instrumentation and fusion may be extended to L4 to reduce the risk of implant failure. However, most authors prefer to perform a circumferential fusion to reduce the risk of pseudoarthrosis. In cases where the lumbosacral kyphosis is irreducible, a trans-sacral fixation can be performed with the use of a fibular strut graft, metallic cages or trans-sacral L5-S1 pedicle screw fixation (Fig. 4-4). The trans-sacral fixation can be performed using an anterior approach such as in a Kellogg-Speed fusion or with a posterior approach using a Bohlman’s fusion using a fibular strut graft.29,30 Such interbody fusion procedures using fibular strut grafts, reduce the risk of pseudoarthrosis following an isolated posterolateral fusion and in-situ fusion. Postoperatively the patient can be placed in a pantaloon brace for a period of 6-8 weeks.
Surgical techniques for trans-sacral delta fixation
An alternative technique for in-situ fusion is a trans-sacral delta fixation.31 In this technique a standard posterior exposure is used to expose from L4 to S1. Pedicle screws are placed in the L4 and L5 bilaterally. The S1 screw entry is taken in a standard fashion; however, the screw trajectory is planned to extend beyond the anterior sacral cortex and into the L5 vertebral body (Fig. 4-5). The length of such transvertebral S1 screw is usually between 60-70 mm.
Surgical technique for trans-sacral fibular strut grafting
In-situ fusion techniques may be aided with fibular strut graft placed in a trans-sacral position. A posterior exposure is performed, and pedicle screws are placed in bilaterally L4, L5 and S1. Under fluoroscopy guidance, an entry point is taken medial and inferior to the S1 pedicle. A trans-sacral trajectory is developed across into the L5 vertebral body. The tract is made using an awl and is serially increased in diameter using a power drill. Fibular strut graft is harvested and prepared to the appropriate size in diameter and length to the tract and impacted into position.
Reduction and fusion
Reduction of the spondylolisthesis is preferred in pediatric high-grade slips as the realignment of the slip helps reduce the stress incurred by the growing bone at the lumbosacral junction. In adults, however, there is controversy with regards to need for reduction in high grade slips. The proponents of reduction suggest numerous advantages favoring reduction. The reduction places the fusion mass in a biomechanical advantage of compression rather than tension, thus resulting in lower pseudoarthrosis rates. The reduction maneuver increases the surface areas in contact, proving a larger fusion bed. The reduction of slip improves the sagittal alignment, improving the cosmetic deformity frequently associated with such severe slips. There is improvement in the gait pattern and reduction in the hamstring spasm with correction of the pelvic retroversion.
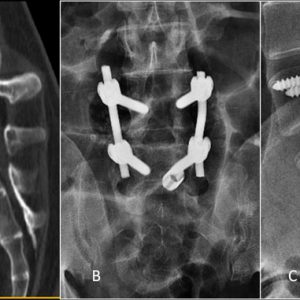
The risks of reduction include a higher chance of neurological deficit and this frequently occurs in the terminal 50% of slip reduction.32 This observation has resulted in some authors advocating partial reduction of slip with circumferential fusion as an acceptable alternative33 (Fig. 4-6). Partial reduction and fusion has been advocated in patients with high grade slip that is accompanied by significant global spinal imbalance or unbalanced pelvis. Partial reduction has lower risk of developing neurological deficit by avoiding significant stretch of the L5 and L4 nerve roots.
Reduction techniques for high grade spondylolisthesis have been described by Ruf et al. and Shufflebarger et al.12,13 Both the techniques suggested by the authors include a temporary screw placement in L4 to achieve distraction and partial reduction of L5. Further reduction in slip and kyphosis is done after performing a wide laminectomy to decompress the L5 roots. By performing a sequential L5-S1 interbody space preparation and use of lordotic cages, further reduction in the slip is achieved (Fig. 4-7). Min et al. suggested that resection of the sacral dome is imperative prior to attempting a reduction as the sacral dome provides a physical obstruction to the reduction of L5 onto the sacrum.34
Basis of reduction and fusion
The Spine Deformity Study Group (SDSG) has developed a classification that offers treatment guidelines to perform reduction in high grade spondylolisthesis.22 The pelvis in high grade spondylolisthesis can be considered to be balanced when the sacral slope is high and pelvic tilt is low. In the scenario of a balanced pelvis, the global spine balance is invariably normal and fusion without reduction is justified. However, in the scenario of an unbalanced pelvis which shows a low sacral slope and high pelvic tilt, a reduction with fusion is indicated.
In this scenario due to the significant retroversion of the pelvis, the global sagittal alignment is affected, and the spine is frequently unbalanced. There is a need to reduce the lumbosacral kyphosis. Reduced pelvic tilt and a partial reduction in the translation can restore the spinal sagittal balance.
Surgical technique for reduction of high grade spondylolisthesis
Operative position
A successful reduction needs meticulous attention to positioning. Prone positioning may result in partial reduction of slip. The aim of preoperative positioning is to reduce the lumbosacral kyphosis thus, aiding in the reduction of the slip. This can be achieved by extending the hip after the patient has been positioned prone. The knees should be flexed to reduce the tension on the L4 and L5 nerve root which are stretched in the process of reduction of the slip.
Surgical techniques
Posterior midline exposure is performed and L4 to S1 posterior elements are exposed. Care is taken to avoid inadvertent damage to the facet capsule at the L4-5 segment. Due to the lumbosacral kyphosis, pedicle screw placement in the L5 vertebra can be difficult. Pedicle screws are placed in L4, S1 and a rod is connected. Distraction over the L4-S1 pedicle screws can help reduce the lumbosacral kyphosis making pedicle screw insertion in L5 easier.
The L5 pedicles are frequently dysplastic, and an accurate screw placement in the L5 is a prerequisite to achieve a successful reduction of the slip. Preferably a bicortical screw purchase in the L5 vertebra is required. Fluoroscopy guided L5 screw placement is recommended to reduce the chances of misplacement.
Prior to any attempt of reduction is performed, it is mandatory that an adequate decompression of the nerve roots are performed to reduce the risk of any neurological deficit. The reduction of lumbosacral kyphosis improves the pelvic tilt and sagittal balance. The reduction in the percentage of slip increases the surface area available for fusion. The dome of the sacrum may need to be resected to help in reduction of the slip.
Postoperative management
Following reduction of high grade slips, frequent neurological examination is required to identify any deficit in the L4 and L5 roots. The hips and knees are positioned in flexion to reduce the stretch on the L4 and L5 nerve roots. Progressive extension of the hip and knee are allowed over a period of 2 weeks keeping a watch for any new onset deficit or radicular symptoms. A brace with extension to the thigh is prescribed for a period of 6 weeks.
Complications
Reduction of high grade spondylolisthesis is known to result in nerve root injury especially in the L5 and L4 roots. This is due to the stretch placed on the root during the process of reduction of the slip. An adequate decompression of the nerve roots and a gradual extension of the hip and knee in the postoperative period can prevent this complication. Due to the pelvic retroversion, the S1 screws may be close to the skin surface and can cause a breakdown of the skin over the prominent implants. Pediatric deformity screws or low head-profile screws can be used to avoid this complication.
Surgical management of spondyloptosis
Surgical treatment of spondyloptosis has been described by Gaines et al.25 The Gaines procedure is a complex two stage vertebral column resection and reconstruction where the spondyloptic L5 vertebra is excised and the L4 is reduced on the S1. In the first stage using an anterior approach the L5 vertebral body, L4-5 disc and L5-S1 disc is resected. Following which, a second stage posterior procedure is performed to excise the L5 pedicles and the posterior elements to eventually allow the reduction of L4 over the S1.
PEARLS AND PITFALLS
- Asymptomatic high-grade spondylolisthesis in adults can be observed closely with non-operative treatment. However, pediatric and adolescent high-grade slips need surgical intervention to counter the risk of slip progression
- Formation defects of the L5 posterior elements, trapezoidal L5 vertebral body, dome shaped S1 vertebral body, high slip angle and pediatric age group are risk factors for progression of spondylolisthesis.
- Clinically high-grade spondylolisthesis can present with L5 radiculopathy, chronic low back pain, cosmetic deformity and neurological deficit involving the cauda equina.
- Surgeon should be aware of possibility of dysplastic pedicles, and this needs a meticulous evaluation with CT scans prior to surgical procedure.
- Spine deformity study group classification can be used as a guide to decide on the need for reduction of high grade slips based on the presence of unbalanced pelvis and global sagittal imbalance.
- Circumferential fusion procedures are preferred to reduce the risk of pseudoarthrosis, though long term clinical and functional results with posterolateral fusion still remain comparable to circumferential fusion surgery.
- In-situ fusion may be considered in patients with a balanced pelvis, acceptable global sagittal balance, no neurological symptoms and large L5 transverse process dimensions. In-situ fixation can be augmented with a fibular strut graft or trans-sacral screw fixation.
- Partial reduction may be preferred over a complete reduction to decrease the risk of post reduction neurological deficit.
REFERENCES
- Burkus JK, Lonstein JE, Winter RB, Denis F. Long-term evaluation of adolescents treated operatively for spondylolisthesis. A comparison of in situ arthrodesis only with in situ arthrodesis and reduction followed by immobilization in a cast. J Bone Joint Surg Am. 1992;74(5):693-704.
- Freeman BL 3rd, Donati NL. Spinal arthrodesis for severe spondylolisthesis in children and adolescents. A long-term follow-up study. J Bone Joint Surg Am. 1989;71(4):594-598.
- Molinari RW, Bridwell KH, Lenke LG, Ungacta FF, Riew KD. Complications in the surgical treatment of pediatric high-grade, isthmic dysplastic spondylolisthesis. A comparison of three surgical approaches. Spine (Phila Pa 1976). 1999;24(16):1701-1711.
- Muschik M, Zippel H, Perka C. Surgical management of severe spondylolisthesis in children and adolescents. Anterior fusion in situ versus anterior spondylodesis with posterior transpedicular instrumentation and reduction. Spine (Phila Pa 1976). 1997;22(17):2036-2042; discussion 2043.
- Cheung EV, Herman MJ, Cavalier R, Pizzutillo PD. Spondylolysis and spondylolisthesis in children and adolescents: II. Surgical management. J Am Acad Orthop Surg. 2006;14(8):488-498.
- DeWald CJ, Vartabedian JE, Rodts MF, Hammerberg KW. Evaluation and management of high-grade spondylolisthesis in adults. Spine (Phila Pa 1976). 2005;30(6 Suppl):S49-59.
- Harris IE, Weinstein SL. Long-term follow-up of patients with grade-III and IV spondylolisthesis. Treatment with and without posterior fusion. J Bone Joint Surg Am. 1987;69(7):960-969.
- Lonstein JE. Spondylolisthesis in children. Cause, natural history, and management. Spine (Phila Pa 1976). 1999;24(24):2640-2648.
- Sailhan F, Gollogly S, Roussouly P. The radiographic results and neurologic complications of instrumented reduction and fusion of high-grade spondylolisthesis without decompression of the neural elements: a retrospective review of 44 patients. Spine (Phila Pa 1976). 2006;31(2):161-169; discussion 170.
- Seitsalo S, Osterman K, Hyvärinen H, Schlenzka D, Poussa M. Severe spondylolisthesis in children and adolescents. A long-term review of fusion in situ. J Bone Joint Surg Br. 1990;72(2):259-265.
- Helenius I, Lamberg T, Osterman K, et al. Posterolateral, anterior, or circumferential fusion in situ for high-grade spondylolisthesis in young patients: a long-term evaluation using the Scoliosis Research Society questionnaire. Spine (Phila Pa 1976). 2006;31(2):190-196.
- Shufflebarger HL, Geck MJ. High-grade isthmic dysplastic spondylolisthesis: monosegmental surgical treatment. Spine (Phila Pa 1976). 2005;30(6 Suppl):S42-48.
- Ruf M, Koch H, Melcher RP, Harms J. Anatomic reduction and monosegmental fusion in high-grade developmental spondylolisthesis. Spine (Phila Pa 1976). 2006;31(3):269-274.
- Bartolozzi P, Sandri A, Cassini M, Ricci M. One-stage posterior decompression-stabilization and trans-sacral interbody fusion after partial reduction for severe L5-S1 spondylolisthesis. Spine (Phila Pa 1976). 2003;28(11):1135-1141.
- Bridwell KH. Surgical treatment of high-grade spondylolisthesis. Neurosurg Clin N Am. 2006;17(3):331-338.
- Transfeldt EE, Mehbod AA. Evidence-based medicine analysis of isthmic spondylolisthesis treatment including reduction versus fusion in situ for high-grade slips. Spine (Phila Pa 1976). 2007;32(19 Suppl):S126-129.
- Rodriguez-Olaverri JC, Zimick NC, Merola A, et al. Comparing the clinical and radiological outcomes of pedicular transvertebral screw fixation of the lumbosacral spine in spondylolisthesis versus unilateral transforaminal lumbar interbody fusion (TLIF) with posterior fixation using anterior cages. Spine (Phila Pa 1976). 2008;33(18):1977-1981.
- Poussa M, Remes V, Lamberg T, et al. Treatment of severe spondylolisthesis in adolescence with reduction or fusion in situ: long-term clinical, radiologic, and functional outcome. Spine (Phila Pa 1976). 2006;31(5):583-590; discussion 591-592.
- Poussa M, Schlenzka D, Seitsalo S, Ylikoski M, Hurri H, Osterman K. Surgical treatment of severe isthmic spondylolisthesis in adolescents. Reduction or fusion in situ. Spine (Phila Pa 1976). 1993;18(7):894-901.
- Wiltse LL, Newman PH, Macnab I. Classification of spondylolisis and spondylolisthesis. Clin Orthop Relat Res. 1976;(117):23-29.
- Marchetti PC, Bartolozzi P. Classification of spondylolisthesis as a guideline for treatment. In: Bridwell KH, DeWald RL (eds). The Textbook of Spinal Surgery, 2nd ed. Philadelphia: Lippincott-Raven. 1997:1211-1254.
- Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J. 2011;20 Suppl 5:641-646.
- Labelle H, Roussouly P, Berthonnaud E, et al. Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine (Phila Pa 1976). 2004;29(18):2049-2054.
- Labelle H, Roussouly P, Chopin D, Berthonnaud E, Hresko T, O’Brien M. Spino-pelvic alignment after surgical correction for developmental spondylolisthesis. Eur Spine J. 2008;17(9):1170-1176.
- Gaines RW. L5 vertebrectomy for the surgical treatment of spondyloptosis: thirty cases in 25 years. Spine (Phila Pa 1976). 2005;30(6 Suppl):S66-70.
- Edwards CC, Bradford DS. Instrumented reduction of spondylolisthesis. Spine (Phila Pa 1976). 1994;19(13):1535-1537.
- Lamartina C, Zavatsky JM, Petruzzi M, Specchia N. Novel concepts in the evaluation and treatment of high-dysplastic spondylolisthesis. Eur Spine J. 2009;18 Suppl 1:133-142.
- Calancie B, Madsen P, Lebwohl N. Stimulus-evoked EMG monitoring during transpedicular lumbosacral spine instrumentation. Initial clinical results. Spine (Phila Pa 1976). 1994;19(24):2780-2786.
- Bohlman HH, Cook SS. One-stage decompression and posterolateral and interbody fusion for lumbosacral spondyloptosis through a posterior approach. Report of two cases. J Bone Joint Surg Am. 1982;64(3):415-418.
- Hanson DS, Bridwell KH, Rhee JM, Lenke LG. Dowel fibular strut grafts for high-grade dysplastic isthmic spondylolisthesis. Spine (Phila Pa 1976). 2002;27(18):1982-1988.
- Smith JA, Deviren V, Berven S, Kleinstueck F, Bradford DS. Clinical outcome of trans-sacral interbody fusion after partial reduction for high-grade l5-s1 spondylolisthesis. Spine (Phila Pa 1976). 2001;26(20):2227-2234.
- Petraco DM, Spivak JM, Cappadona JG, Kummer FJ, Neuwirth MG. An anatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine (Phila Pa 1976). 1996;21(10):1133-1138; discussion 1139.
- Boachie-Adjei O, Do T, Rawlins BA. Partial lumbosacral kyphosis reduction, decompression, and posterior lumbosacral transfixation in high-grade isthmic spondylolisthesis: clinical and radiographic results in six patients. Spine (Phila Pa 1976). 2002;27(6):E161-168.
- Min K, Liebscher T, Rothenfluh D. Sacral dome resection and single-stage posterior reduction in the treatment of high-grade high dysplastic spondylolisthesis in adolescents and young adults. Eur Spine J. 2012;21 Suppl 6:S785-791.