Jaspreet Johal and R. Shane Tubbs*
OVERVIEW
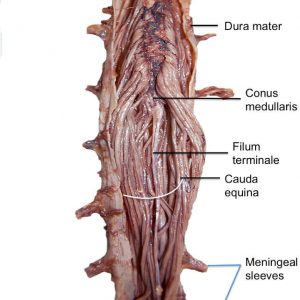
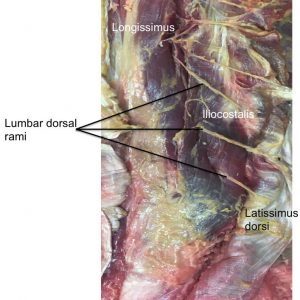
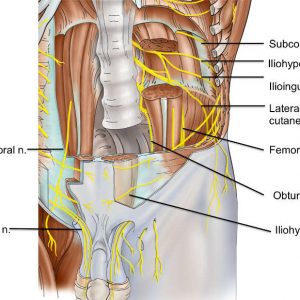
There are many nerves that serve the lumbar region. The spinal cord terminates in this area as the conus medullaris (Fig. 3-1), which in most individuals is located between the L1 and L2 vertebrae. Within the spinal dura mater, the spinal cord and its dorsal and ventral rootlets are covered by arachnoid and pia mater (Fig. 3-2). These rootlets travel laterally (Fig. 3-3) into meningeal nerve sheaths within the intervertebral foramina where they join as a spinal nerve (Fig. 3-4). This short segment (Fig. 3-5) then quickly branches into smaller dorsal rami, which will innervate native back muscles, the facet joints and the skin overlying the back and larger ventral rami, which in the lumbar region will interdigitate to form the lumbar plexus. The dorsal rami (Fig. 3-6) near their exit from the intervertebral foramina will branch into medial, intermediate (variable and sometimes arising from the lateral branch) and lateral branches. The lateral branches are distributed in the lumbar region primarily to the iliocostalis lumborum muscle, although upper lumbar lateral branches do become cutaneous (Fig. 3-7). The intermediate branches travel to the longissimus muscle and the medial branches innervate the facet joints and multifidus muscles. Other branches in this region include the sympathetic trunks (Figs. 3-2 and 3-5), which in the lumbar region travel on the anterolateral surface of the lumbar vertebral bodies and below L1, connecting to adjacent spinal nerves via gray rami communicans. Normally, the L4 ventral ramus will communicate with the L5 ventral ramus to form the lumbosacral trunk that then continues into the pelvis to contribute to the sacral plexus, i.e., lumbosacral plexus.

LUMBAR PLEXUS
The lumbar plexus forms within the psoas major muscle in the retroperitoneal space (Fig. 3-8), and is derived from contributions arising from the first three lumbar ventral rami, along with additional contributions from parts of the fourth lumbar ventral rami and 12th thoracic ventral ramus.
ILIOHYPOGASTRIC NERVE (T12, L1)
The iliohypogastric nerve (Figs. 3-9 and 3-10) forms within the lumbar plexus, and commonly arises from contributions from the 12th thoracic ventral ramus and usually from the first lumbar ventral ramus. It courses past the psoas major and exits from the upper lateral border of the psoas major, at a point between the anterior surface of quadratus lumborum and the posterior aspect of the kidney. The iliohypogastric nerve then traverses past the posterior part of the transversus abdominis, traveling superior to the iliac crest. Near the iliac crest, it divides into anterior and lateral branches between the transversus abdominis and internal oblique. The anterior branch of the iliohypogastric nerve supplies surrounding muscles such as internal oblique, transversus abdominis, and the conjoint tendon while also supplying sensory innervation of the suprapubic skin. The lateral cutaneous branch supplies the posterolateral gluteal skin.1,2 In the presence of a pyramidalis muscle, it is likely to be innervated by the iliohypogastric nerve.
ILIOINGUINAL NERVE (L1)
The ilioinguinal nerve (Figs. 3-9 and 3-10) exists as a collateral branch of the first ventral ramus of the lumbar nerve, and it emerges from along the lateral border of the psoas major alongside or just below the iliohypogastric nerve. It then proceeds down the anterior surface of the quadratus lumborum towards the upper portion of the iliacus. It travels through the transversus abdominis near the iliac crest, and then pierces through the internal oblique to supply it. During its descent it passes 3 cm medial and 3.5 cm inferior to the anterior superior iliac spine. At this point, the ilioinguinal nerve is located in the plane between the internal and external obliques and travels through the inguinal canal. It then exits the superficial inguinal ring on the anterior aspect of the round ligament/spermatic cord. The ilioinguinal nerve goes on to supply sensory innervation of the medial thigh, along with the root of the penis and anterior scrotum in males or the mons pubis and labium majora in females.1
GENITOFEMORAL NERVE (L1, L2)
The genitofemoral nerve (Figs. 3-9 and 3-10) forms within the psoas major from contributions arising from the first and second ventral rami of the lumbar nerve. It is first seen at the anterior surface of the psoas major along its medial border. It then proceeds downward along the psoas major, traveling within the iliac fascia and traveling posteriorly to the ureter and peritoneum. The genitofemoral nerve then travels along the lateral border of the common and external iliac artery, and divides into genital and femoral branches at a point above the inguinal ligament. The genital branch enters the deep inguinal ring by traveling through the transverse and spermatic fascia. It then descends down the inguinal canal deep to the round ligament/spermatic cord and provides innervation of the cremaster muscle. Finally, it exits through the superficial inguinal ring and gives off sensory branches to the lateral aspect of the scrotum in males or the mons pubis and labium majus in females along with surrounding parts of the thigh. The femoral branch of the genitofemoral nerve travels alongside the femoral artery underneath the inguinal ligament and travels through the femoral sheath at a point superficial and lateral to the femoral artery and distal to the inguinal ligament. It then emerges from the sheath and fascia lata to provide sensory innervation of the skin of the upper anterior part of the femoral triangle.3
Variation
The iliohypogastric nerve may be absent from the lumbar plexus in up to 20% of cases. The ilioinguinal nerve is not seen in less than 3% of the population, and in 25% of cases it may emerge with the iliohypogastric nerve. Within the inguinal canal, the ilioinguinal nerve is usually seen anterior to the spermatic cord but it may also lie within or posterior to the cord, or outside the inguinal canal entirely. The genitofemoral nerve arises from two separate branches in 20% of cases, and in some instances either of its branches or the entire nerve may be absent.
General Mechanisms of Injury
The iliohypogastric, ilioinguinal, and genitofemoral nerves may be injured along their course through the anterior and posterior abdominal wall either directly by trauma (e.g., surgical injury or during suture ligation) or indirectly by ischemic damage secondary to reduced perfusion or stretch. These nerves may be most prone to injury during certain portions of their course through the abdomen and surrounding regions. The anterior branch of the iliohypogastric nerve may be most vulnerable to injury during its course through the internal and external obliques. The ilioinguinal nerve appears to be prone to injury during its descent along the anterior abdominal wall, and the genitofemoral nerve is vulnerable to injury throughout its entire course, but this risk is most pronounced in the retroperitoneum and within the inguinal canal.
Context of Injury
These nerves may undergo iatrogenic injury during abdominal and pelvic surgery (e.g., appendectomy, repair of inguinal hernia, gynecologic procedures through transverse incision, femoral artery catheterization, fascial closure, and procedures for urinary incontinence such as needle suspension and tension-free vaginal tape). Surgery to repair an inguinal hernia commonly results in injury to the ilioinguinal nerve. Laparoscopic inguinal hernia repair also may cause injury to the femoral branch of the genitofemoral nerve, whereas open inguinal hernia repair may damage the genital branch. The femoral branch may also be injured during femoral artery catheterization procedures.
Effects of Injury
Clinical manifestations of injury to the iliohypogastric nerve appear to differ based on whether injury occurs above or below the anterior superior iliac spine. In injuries occurring below the anterior superior iliac spine, some loss of sensory innervation of suprapubic skin may be observed – however, this is rarely seen due to collateral sensory innervation of this region. Injuries occurring above the anterior superior iliac spine, however, may weaken muscles such as the internal oblique, transversus abdominis, and conjoint tendon. A direct hernia may form secondary to this loss of muscle innervation. Injury to the ilioinguinal nerve may lead to numbness and parathesia over skin of the genitalia, and entrapment injuries during surgery may lead to the development of recurrent pain along its area of distribution. Injury to the genitofemoral nerve will also produce parathesia and anesthesia along its area of distribution.
LATERAL FEMORAL CUTANEOUS NERVE (L2, L3)
The lateral femoral cutaneous nerve (Figs. 3-9 and 3-10) is derived from contributions arising at the second and third ventral rami of the lumbar nerve, and is seen emerging from the lateral margin of the psoas major. It then proceeds downward and deep to the fascia that covers the iliacus, and passes underneath or less commonly through the inguinal ligament at a point medial to the anterior superior iliac spine. In its course through the thigh, the lateral cutaneous nerve of the thigh initially runs deep to the fascia lata and over the surface of the sartorius muscle. It then pierces through the fascia lata to supply sensory innervation to the lateral aspect of the thigh. At this point, it divides into anterior and posterior branches. The anterior branch serves to provide sensory innervation of skin along the anterolateral thigh and goes on to contribute to the patellar plexus. The patellar plexus is formed by the anterior branch of the lateral cutaneous nerve of the thigh, anterior cutaneous branches of the femoral nerve, and infrapatellar branches of the saphenous nerve. The posterior branch of lateral cutaneous nerve of the thigh provides sensory innervation of skin from the greater trochanter to the middle of the thigh.4,5
Variation
Anatomical variations of the lateral cutaneous nerve of the thigh are observed in around 25% of the population, and the nerve may be completely absent in around 10% of individuals.
General Mechanisms of Injury
The lateral cutaneous nerve of the thigh is most prone to injury either around the inguinal ligament or along the anterior or anterolateral proximal thigh by direct trauma. Commonly indicated mechanisms of injury include iatrogenic injury secondary to incision, transection, or suture ligation along with prolonged use of belts and braces, and accidental trauma. Iatrogenic injury to the lateral cutaneous nerve of the thigh has been reported as the eighth most common cause of iatrogenic injury during surgical procedures.6
Context of Injury
Iatrogenic injury of the lateral cutaneous nerve of the thigh may occur during surgical procedures involving the abdomen and pelvis. Implicated procedures include any involving an anterior or anterolateral approach to the hip, ilioinguinal approach to the acetabulum, inguinal hernia repair, inguinal lymph node biopsy, discectomy, ovarian cystectomy, and femoral artery catheterization performed by radiologists.
Effects of Injury
Injury to the lateral cutaneous nerve of the thigh can result in a spectrum of clinical disabilities that can range from a sensory defect of the lateral thigh to painful neuromas in its area of distribution. Injury to the nerve is implicated in the development of meralgia paresthetica, which is a clinical syndrome characterized by itching, burning, pain, and numbness over the anterolateral aspects of the thigh.
OBTURATOR NERVE (L2, L3, L4)
The obturator nerve (Figs. 3-9 and 3-10) is derived from the anterior divisions of the ventral rami of the second to fourth lumbar nerves. It initially proceeds down the psoas major to appear at the medial side of the psoas major at a point nearby the pelvic brim. This point of emergence is localized medial to the lumbosacral trunk, posterior to the common iliac vessels, and posterolateral to the sacroiliac joint. The obturator nerve then descends down the lateral pelvic wall to exit the pelvis via the obturator foramen. During its course down the lateral pelvic wall, it runs alongside the obturator artery and travels on the obturator internus muscle. At this point, there are several anatomically significant structures that lie in close proximity to the obturator nerve. From posterior to anterior, these structures are the iliac vessels, the ureter, in rare cases a pelvic appendix on the right and a sigmoid colon on the left, the ovary and infundibulum of the Fallopian tube in females and the ductus deferens in males.
As the obturator nerve passes through the obturator foramen, it will divide into anterior and posterior branches. The anterior branch of obturator nerve travels in a plane formed by the adductor longus anteriorly and the adductor brevis posteriorly. A branch of the anterior division supplies the hip joint and the majority of the adductor muscles, and an arterial branch travels to the femoral artery. It also communicates with cutaneous branches of the femoral nerve within the adductor canal, forming the subsartorial plexus and providing innervation of the medial aspect of the thigh. The posterior branch of obturator nerve pierces through the obturator externus and innervates that muscle. It then proceeds downward behind the adductor brevis and travels on to the adductor magnus. The posterior division will innervate the adductor magnus, and may occasionally supply the adductor brevis muscle. It then travels through the adductor hiatus to reach the popliteal fossa, where it transmits an articular branch to the knee joint that runs alongside the middle genicular artery.
Variation
The accessory obturator nerve is a structural anomaly that may be observed in less than 15% of cases. It is commonly formed from contributions arising from the ventral rami of the third and fourth lumbar nerves. This abnormal nerve often traverses past the medial border of the psoas major, crossing past the superior pubic ramus and running behind the pectineus muscle. Depending on its exact trajectory, it may supply the pectineus muscle and/or the hip joint. Its point of origin may be the trunk of obturator nerve, or it may connect with the anterior division of the obturator nerve.7
General Mechanisms of Injury
During its course, the obturator nerve is prone to either direct injury as a result of trauma (e.g., compression, iatrogenic damage during incision or transection, or accidental) or indirect injury secondary to ischemic damage. Some mechanisms such as a pelvic mass (e.g., ovarian tumor or obturator hernia) may produce both direct traumatic and indirect ischemic injury. The most vulnerable aspect of this nerve is the intrapelvic segment.
Context of Injury
Iatrogenic injury of the obturator nerve may occur during abdominopelvic procedures, hip joint repair, regional anesthesia delivery, and urological surgery. Implicated procedures include radical prostatectomy, total hip arthroplasty, labor and delivery of a neonate, abdominal aortic aneurysm repair, and obturator hernia repair.
Effects of Injury
Obturator nerve injury may produce pain and sensory abnormalities of the medial thigh and these symptoms may occasionally extend to below the knee. Loss of sensory innervation may be limited as its area of distribution overlaps with neighboring cutaneous branches. Loss of motor innervation may result in atrophy of muscles within the medial thigh, but impaired functionality will be limited to the adductor magnus muscle. This will result in muscle disability characterized by limited adduction, which will not impact walking but may make crossing of the legs more difficult.
FEMORAL NERVE (L2, L3, L4)
The femoral nerve (Figs. 3-9 and 3-10) forms within the lumbar plexus with contributions arising from the posterior division of the ventral rami from the second to fourth lumbar nerves. It first exits from along the lateral border of the psoas major within the iliac fossa at a point around 4 cm above the inguinal ligament. The femoral nerve then enters the femoral triangle passing laterally by the femoral sheath, and within a few centimeters of its entry into the femoral triangle it divides into anterior and posterior divisions. Within the thigh, the femoral nerve gives off a number of sensory and muscular branches, and its sole branch, the saphenous nerve, goes on to course below the knee.
Within the iliac fossa, the femoral nerve courses alongside the external iliac artery as it exits the abdomen. It runs posterior to the ileocecal portion of the bowel on the right and posterior to the sigmoid colon on the left. The femoral nerve gives off small branches to the femoral artery and iliacus muscle within the iliac fossa. It also innervates the pectineus muscle, with these branches arising variably from either the abdomen or thigh. As it enters the femoral triangle, the femoral nerve runs lateral to the femoral sheath and the vessels within it, segregated from them by psoas fibers. It lies upon the iliacus with the fascia lata serving as the roof of the femoral triangle. After giving off a number of small branches, the femoral nerve then divides into anterior and posterior divisions at a point about 1–4 cm below the inguinal ligament. These divisions may often be separated by the lateral circumflex femoral artery, or this artery could lie deep to both divisions.8
The anterior division of the femoral nerve is relatively short and immediately gives off a branch to the sartorius and two sensory branches after forming below the inguinal ligament. The two sensory nerves are the intermediate and medial cutaneous nerves of the thigh.
The intermediate cutaneous nerve of the thigh travels through the fascia lata at a point about 8 cm below the inguinal ligament and further divides into two branches. These branches then descend down the thigh and innervate the skin down to the knee, where they contribute to the peripatellar plexus. The more laterally located of these two branches communicates with the femoral branch of the genitofemoral nerve and may also supply the sartorius muscle.
The medial cutaneous nerve of the thigh descends laterally past the femoral artery and gives off small branches that pierce through the fascia lata and provide innervation to the superior part of the medial thigh. At the apex of the femoral triangle, the medial cutaneous nerve of the thigh will pass anterior to the femoral artery and divide into anterior and posterior branches. The anterior branch descends down the sartorius and pierces through the fascia lata at around the middle length of the thigh, where it further divides into two branches. One of these branches supplies the skin of the medial knee and the other connects with the infrapatellar branch of the saphenous nerve. The posterior branch travels down the posterior border of the sartorius to the knee, where it goes through the fascia lata and connects with the saphenous nerve. It goes on to contribute to the subartorial plexus and also provide innervation to the medial aspect of the leg just below the knee.
The posterior division of the femoral nerve gives off the saphenous nerve and also provides innervation to the quadriceps femoris and articularis genus. The saphenous nerve exists as an entirely cutaneous branch of the femoral nerve. In the groin it runs lateral to the femoral artery before crossing over to the medial side via the adductor canal. As it leaves the adductor canal alongside the saphenous branch of the descending genicular artery, the saphenous nerve gives off an infrapatellar branch that pierces the sartorius and supplies skin surrounding the knee. It then descends further downward to pierce the fascia lata between the tendons of the sartorius anteriorly and gracilis posteriorly, and communicates with the great saphenous vein at a point behind the medial aspect of the knee. It travels alongside the vein in the leg and divides into two branches at a variable point.9 The larger of these branches, the anterior branch, courses alongside the great saphenous vein at the medial surface of the tibia and goes on to supply skin on the medial aspect of the foot down to the first metatarsophalangeal joint. The posterior branch descends down the medial border of the tibia to terminate at the ankle and supply cutaneous sensation to the medial aspect of the leg.
Muscular branches of the posterior division of the femoral nerve supply the rectus femoris, vastus lateralis, vastus medialis, vastus intermedius, and articularis genus. The branch to the rectus femoris enters through the posterior surface of the muscle and also supplies the hip joint. The vastus lateralis is supplied by a larger branch that descends alongside the lateral circumflex femoral artery and enters the muscle through its anterior border while also supplying the knee joint. An even larger branch supplies the vastus medialis and is seen to travel alongside the femoral vessels and saphenous nerve within the adductor canal. It gives off branches to upper and lower segments of the muscle and also sends a long filamentous branch to the knee. A few branches to the vastus intermedius enter through that muscle’s anterior surface at around the mid-thigh level and a small branch descends to supply the articularis genus and the knee joint.
The femoral nerve is supplied by the iliolumbar artery within the pelvis, by the deep circumflex iliac artery in the inguinal area, and by the lateral circumflex femoral artery within the thigh. On the right side, the deep circumflex iliac artery gives more arterial branches to the femoral nerve relative to the left side, and also forms a richer anastomosis with the iliolumbar and fourth lumbar arteries. The left femoral nerve is therefore more prone to ischemic injury than the right side. The intrapelvic segment of the nerve also appears to be more vulnerable to ischemia than other segments of the nerve.10
Variations
Around 1/3 of individuals appear to show some degree of variability in femoral nerve anatomy. Of these variations, the only one of any clinical significance is within the femoral triangle where the nerve is reported to enter the thigh at some point between the femoral artery and femoral vein.11
General Mechanisms of Injury
The femoral nerve can be involved in both open and closed injury resulting from penetrating trauma and gunshot wounds, blunt trauma, and injury secondary to disease and iatrogenic causes. Penetrating trauma can cause injury at any point along the course of the femoral nerve, but is most likely to occur during wounding of the anterior aspect of the femoral triangle. Blunt injury may occur following an automobile accident, sports injury, or a severe fall. Injury can also occur directly through trauma (e.g., transection following pubic fracture) or secondary to ischemic damage following stretch or impaired perfusion (e.g., hemorrhage into the iliacus compartment following rupture of iliacus or iliopsoas). Some disease processes may damage the nerve directly via inflammation and toxic injury or indirectly due to ischemic damage (e.g., tumors, renal or appendiceal abscess, and hemorrhagic diseases).
Context of Iatrogenic Injury
Iatrogenic injury of the femoral nerve can be reported after procedures involving the abdomen and pelvis, hip surgery, femoral artery puncture, and delivery of regional anesthesia.12 Several causes of nerve injury exist during procedures of the abdomen and pelvis, including compression, ischemia, and direct injury from utilization of surgical instruments. Risk factors for iatrogenic injury include thin or obese body habitus, and the use of Pfannenstiel incisions. Compression injuries usually occur during the use of retractors, as they may compress the nerve against the pelvic wall or the tip of the blade may directly exert pressure on the nerve. Stretching and compression of the femoral nerve may also occur during procedures in which a patient is placed in a lithotomy position with extreme flexion, abduction, and external rotation of the thighs for a prolonged period of time. During this positioning, the femoral nerve can become sharply angulated underneath the inguinal ligament. Nerve compression can also occur due to formation of a hematoma in anticoagulated patients undergoing vascular procedures.12
The femoral nerve can also experience iatrogenic damage during orthopedic procedures, especially those involving lateral and anterolateral approaches to the hip joint. Causes of femoral nerve injury during hip surgery include: (i) prolonged or extreme retraction of the nerve during surgery by instruments, bone, or prosthesis; (ii) compression and stretching from hyperextension and limb lengthening; (iii) formation of a hematoma around the femoral vein or iliacus; (iv) cement extrusion; and (v) laceration or transection.12 Iatrogenic injury can also occur during delivery of regional anesthesia, particularly during a femoral nerve block. The etiology appears to be direct needle penetration of the nerve due to ischemia, intraneural injection, and neural toxicity caused by large doses of local anesthetic agent.12
Transient neuropathy of the femoral nerve has also been reported during the use of regional anesthesia during inguinal hernia repair and iliac crest bone harvest. This occurs because anesthetic agents delivered into the plane between the transversus abdominis and the transversalis fascia can easily diffuse posteriorly into the space between the iliacus and its overlying fascia, where the femoral nerve is located.13 The femoral nerve can also be injured when blood is obtained from the femoral artery for arterial blood gas analysis or angiography through the femoral artery. This occurs either due to direct injury or indirectly due to compression from hematoma or pseudoaneurysm.
Injury to the saphenous nerve may be the subject of surgical management, as the nerve may be sectioned or damaged during surgical procedures. Iatrogenic injury to the saphenous nerve has commonly been reported during total stripping of the great saphenous vein. This is due to the course of the nerve and the close proximity in which it follows the vein below the knee. It has also been reported that the saphenous nerve can be compressed on the operating table due to improper application of supporting braces. Iatrogenic injury has been reported during utilization of peripheral nerve blocks as well, however there appears to be no indication of saphenous nerve injury secondary to adductor canal blockade.14
Effects of Injury
The femoral nerve is most vulnerable to injury at the lower abdomen and upper thigh due to its relatively superficial course in that region and its close proximity to the acetabular rim. It may also be compressed by tumors or hematomas within the pelvis. Severe injury to the femoral nerve within the pelvis may result in weakness of ipsilateral hip flexion, knee extension, sensory impairment over the anterior thigh and medial aspect of leg and foot, loss of knee jerk reflex, and atrophy of the quadriceps with loss of patellar reflex. Destabilization of the lower limb can lead to difficulty performing activities such as walking uphill or on uneven ground and climbing stairs. Sensory impairments seen are limited to hyperesthesia, paresthesia, numbness over the anteromedial aspect of the thigh and leg, and pain in the thigh or groin.
Injury to the femoral nerve occurring within the thigh can produce a range of clinical presentations, including complete or isolated motor or sensory deficit. Physical symptoms include reduced or completely absent patellar reflex, and partial or complete atrophy of the quadriceps. An incomplete lesion of the femoral nerve may be indicated by sweating within its autonomous cutaneous distribution. Lesions of the femoral nerve may be more common on the left side than on the right due to relatively less blood supply on the left.10 Patients who experience a postoperative fall with subsequent alteration and impairment of cutaneous sensation in the distribution of femoral nerve should be examined for femoral nerve injury.15 Injury to the saphenous nerve will result in sensory disturbances over the medial aspect of the leg extending along the inner border of the foot to the big toe.
SUGGESTED READINGS
- Bogduk N. Clinical and Radiological Anatomy of the Lumbar Spine. 5th ed. Philadelphia: Elsevier; 2012.
REFERENCES
- Klassen Z, Marshall E, Tubbs RS, Lois RJ Jr., Wartmann CT, Loukas M. Anatomy of the ilioinguinal and iliohypogastric nerves with observations of their spinal nerve contributions. Clin Anat. 2011;24(4):454-461.
- Wijsmuller AR, Lange JF, Kleinrensink GJ, et al. Nerve-identifying inguinal hernia repair: a surgical anatomical study. World J Surg. 2007;31(2):414-420.
- Rab M, Ebmer J, Dellon AL. Anatomic variability of the ilioinguinal and genitofemoral nerve: implications for the treatment of groin pain. Plast Reconstr Surg. 2001;108(6):1618-1623.
- Aszmann OC, Dellon ES, Dellon AL. Anatomical course of the lateral femoral cutaneous nerve and its susceptibility to compression and injury. Plast Reconstr Surg. 1997;100(3):600-604.
- Carai A, Fenu G, Sechi E, Crotti FM, Montella A. Anatomical variability of the lateral femoral cutaneous nerve: findings from a surgical series. Clin Anat. 2009;22(3):365-370.
- Moore AE, Zhang J, Stringer MD. Iatrogenic nerve injury in a national no-fault compensation scheme: an observational cohort study. Int J Clin Pract. 2012;66(4):409-416.
- Katritsis E, Anagnostopoulou S, Papadopoulos N. Anatomical observations on the accessory obturator nerve (based on 1000 specimens). Anat Anz. 1980;148(5):440-445.
- Orebaugh SL. The femoral nerve and its relationship to the lateral circumflex femoral artery. Anesth Analg. 2006;102(6):1859-1862.
- Wilmot VV, Evans DJ. Categorizing the distribution of the saphenous nerve in relation to the great saphenous vein. Clin Anat. 2013;26(4):531-536.
- Boontje AH, Haaxma R. Femoral neuropathy as a complication of aortic surgery. J Cardiovasc Surg (Torino). 1987;28(3):286-289.
- Bergman RA, Thompson SA, Afifi AK. Catalog of Human Variation. Baltimore: Urban & Schwarzenberg; 1984, p. 159.
- Moore AE, Stringer MD. Iatrogenic femoral nerve injury: a systematic review. Surg Radiol Anat. 2011;33(8):649-658.
- Rosario DJ, Jacob S, Luntley J, Skinner PP, Raftery AT. Mechanism of femoral nerve palsy complicating percutaneous ilioinguinal field block. Br J Anaesth. 1997;78(3):314-316.
- Henningsen MH, Jaeger P, Hilsted KL, Dahl JB. Prevalence of saphenous nerve injury after adductor-canal-blockade in patients receiving total knee arthroplasty. Acta Anaesthesiol Scand. 2013;57(1):112-117.
- Feibel RJ, Dervin GF, Kim PR, Beaule PE. Major complications associated with femoral nerve catheters for knee arthroplasty: a word of caution. J Arthroplasty. 2009;24(6 Suppl):132-137.

