- See: Trauma Menu
- Discussion:
- note that with acetabular fracture associated with major trauma that there will be 50% chance of
at least one other major injury;
- neuro and head injury (see Glasgow)
- abdominal and chest injury (pulmonary contussion and pneumothorax);
- genito-urinary injury
- spine
- spinal injury
- pelvic fracture may occur in approx 20 % of acetabular frx;
- frx dislocation of the hip:
- Surgical treatment and prognosis of acetabular fractures associated with ipsilateral femoral neck fractures.
- extremity injury
- knee injuries: PCL rupture and/or patella frx;
- ref: Knee Injury Associated With Acetabular Fractures: A Multicenter Study of 1273 Patients.
- vascular injuries:
- fluid management and need for transfusion are kept in mind as soon as the patient arrives in the ER;
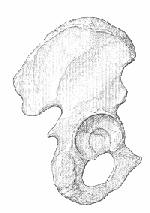
- Radiographs:
- classification
- Physical Exam:
- inspection of soft tissues:
- including local wounds, abrasions, & closed degloving injury;
- Morel Lavale lesion;
- closed degloving injury which commonly occurs over greater trochanter;
- subQ tissue is torn from fascia creating a cavity, which places this tissue at risk for infection and/or poor healing;
- reference:
- Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: the Morel-Lavallée lesion.
- palplation:
- symphysis, pubic rami, iliac crests, sacroiliac;
- bimanual compression & distraction of the iliac wings, & abduction & adduction of the hip should be done to detect instability;
- manual traction can aid in the determination of vertical instability
- GYN / urinary / rectal injuries: RUG vs. suprapubic catheter placement;
- neurologic injury:
- a careful detailed examination of the sciatic nerve is manditory in all cases;
- w/ posterior injury, the sciatic nerve may be injured in 40% of patients;
- references:
- Knee Injury Associated With Acetabular Fractures: A Multicenter Study of 1273 Patients.
- Indications for Non Operative Rx:
- may be indicated if the superior acetabular dome is intact, based on the 3 standard roof arc measurements (which
should be greater than 45 deg);
- indicated for both column frx which are congruent and which dont have wide displacement, as determined by 3 arc measurements;
- posterior acetabular wall should be adequate;
- low transverse frx not involving wt bearing dome;
- many low anterior column frx that involve only pubic portion of acetabulum can be treated by non operative means;
- minority of low T shaped or transverse frx can be treated non-op;
- if non surgical treatment is selected, Neufield type roller traction has the advantage of permitting active lower extremity exercises;
- traction must be maintained from 4-8 weeks to achieve bony union;
- in the presentation by Stover M, et al (1999), the authors were able to follow 33 patients with minimally displaced
acetabular frx w/o surgery;
- non displaced frx were defined as displacement less than 1 mm, and minimally displaced frx had less than 2 mm of
displacement;
- the majority of fractures were of the transverse type;
- 31 out of 33 fractures healed without fracture displacement;
- non of the 13 nondisplaced fractures displaced when patients were allowed touch down wt bearing;
- advocate early touch down mobilization for minimally displaced acetabular frx, as long as there is close radiographic follow up;
- ref: Nonop treatment of fractures of the acetabulum. Stover M, et al. (15th Annual Meeting of the OTA);
- Surgical Treatment:
- indications for ORIF acetabular fractures
- articular displacement of more than 2 mm or persistent displacement following closed reduction (and traction);
- a nonconcentric reduction after dislocation of the hip out of traction (on any radiographic view);
- any intraarticular loose bodies associated w/ acetabular fracture
- unstable fracture of posterior acetabular wall;
- lack of parallelism between femoral head and acetabular roof;
- medial femoral head subluxation;
- instability out of traction after closed reduction;
- total hip replacement
- contraindications to surgery
- acute fixation in polytrauma is avoided unless an ipsilateral hip fracture is present;
- open fractures;
- severe injuries to adjacent skin (Morel Lavale lesion);
- bladder rupture
- fever
- osteoporosis
- Pre Op Planning:
- timing:
- ideal time to perform surgery is between 2 and 10 days after injury;
- delay of 2-3 days is desirable to help decrease local intraop bleeding;
- beyong 10 days, frx fragments are not as easily manipulated;
- after 3 weeks delay callus can complicate frx reduction;
- associated injuries:
- pts must be afebrile and off ATB for > 48 hrs prior to surgery;
- prior to surgical intervention, all other injuries are stabilized;
- physical exam:
- inspection of soft tissues:
- GYN / urinary / rectal injuries:
- neurologic injury: it is essential that all neurologic deficits are documented prior to surgery;
- vascular injuries: (see vascular injuries in pelvic frx)
- injury to the superior gluteal artery may lead to flap necrosis in patients undergoing iliofemoral (or other extensile exposures);
- acetabular fractures which are displaced into the sciatic notch should undergo preoperative angiography;
- references:
The Superior Gluteal Artery in Complex Acetabular Procedures. A Cadaveric Angiographic Study.
Preoperative angiographic assessment of the superior gluteal artery in acetabular fractures requiring extensile surgical exposures.
- traction:
- pts are maintained in skeletal traction preoperatively, & reduction of the femoral head is confirmed roentgenographically;
- usually intraop traction is employed either through the distal femoral pin and fracture table, or an ASIF femoral distractor;
- deep venous thrombosis;
- consider placement of inferior vena cava - DVT filter;
- consider heparin or coumadin;
- blood loss:
- expect intra-operative blood loss of 1500-3500 cc;
- type and cross 3-4 units of pRBC
- consider use of a cell saver;
- flourscopy:
- if flouroscopy is required, avoid using Nitrous oxide anesthesia since it obscurs bony details;
- ensure that there is no contrast material in the patients GI tract or bladder;
- Surgical Approaches:
- Iliofemoral Approach
- Ilioinguinal Approach
- used for frx of anterior wall, anterior column, anterior column- posterior hemitransverse frx, and both column frx;
- Kocher Langenbach:
- used for fractures of posterior wall, posterior column, combined frx of the posterior wall and column, T shaped frx;
- w/ T fractures, the Kocher Langenback is used most often, unless the frx courses from proximal-anterior to distal-posterior
w/ anterior displacement in which case the ilio-inguinal approach should be selected;
- Complications:
- post traumatic DJD
- A Sobering Message to Acetabular Fracture Surgeons: Commentary on an article by Diederik O. Verbeek, MD, et al.: "Predictors for Long-Term Hip Survivorship Following Acetabular Fracture Surgery. Importance of Gap Compared with Step Displacement".
- Predictors for Long-Term Hip Survivorship Following Acetabular Fracture Surgery: Importance of Gap Compared with Step Displacement.
- infection
- sciatic nerve palsy
- can be prevented by flexion of the knee during surgery and intraop monitoring of amount of tension applied by assistants
retracting the nerve;
- early treatment consists of AFO
- sciatic nerve recovery may occur over a 3 yr period;
- tendon transfers are usually not performed unitl 3 yr post op;
- reference: Sciatic Nerve Release Following Fracture or Reconstructive Surgery of the Acetabulum
- deep venous thrombosis
- heterotopic ossificaiton:
- heterotopic ossification is rare w/ non operative treatment;
- w/ operative treatment and no prophylaxis, HO may occur in 90%, and will be especially severe in 20-50%;
- clinically significant HO occurs in about 7-14% of surgically treated acetabular fractures;
- typically the maximum amount of HO appears by 3 months;
- some controversy as to whether indomethacin actually reduces HO;
- in the study by Matta and Siebenrock (1997), indomethacin was not effective for preventing ectopic bone formation;
- risk factors:
- iliofemoral approach (HO occurs in 57%)
- Kocher Langenbeck approach (HO occurs in 26.3%)
- Ilioinguinal approach (HO occurs in 4.8%)
- multiple trauma, head injury, T-type fracture;



- NSAIA:
- indomethacin 25 mg PO tid for 3-6 months;
- some controversy as to whether indomethacin actually reduces HO;
- in the study by Matta and Siebenrock (1997), indomethacin was not effective for preventing ectopic bone formation;
- in the report Burd TA, et al (2001), the authors studied 166 acetabular frx patients;
- patients were randomized to receive either radiation (800 cGy within 72 hrs of surgery or indocin 25 PO tid;
- grade III or IV HO developed in 11% of indocin group and 4% in the radiation group;
- in 16 patients that did not receive prophylaxis, all develped HO and 6/16 (38%) developed grade III or IV HO;
- etidronate
- radiation therapy
- references:
- Does indomethacin reduce heterotopic bone formation after operations for acetabular fractures? A prospective randomised study.
- Indomethacin compared with localized irradiation for the prevention of heterotopic ossification following surgical treatment of acetabular fractures.
- Post Operative Management:
- passive motion is initiated after drain removal and crutch walking w/ 15 kg wt bearing starts as soon as pain is diminished, usually
two to five days postoperatively;
- 8 weeks after internal fixation, wt bearing is increased progressively, assuming the fracture shows evidence of healing;
- Frx - Menu
- Axial Skeleton:
- C-spine
- Spine
- Pelvis
- distal femoral traction for reduction;
- Neuro:
- document any preoperative neurological deficits;
- Cranio-Maxillo-Facial
- Spine
- Cardiac
- Pulmonary
- GU/Renal
- suprapubic vs. foley catheter (consider RUG)
- Vascular
- see Bleeding w/ Pelvic Frx;
- selective angiography may aid in the dx of of superior gluteal artery;
especially if frx involves sciatic notch;
- if one is using the anterior or posterior approaches to acetabulum using trochanteric osteotomy, superior gluteal vessels
must be intact in order to avoid muscle necrosis of medius and minimus;
- Compartments
- Hepatic / GI tract:
- need for diversion w/ open fractures;
- Coag
- consider Greenfield filter for DVT prophylaxis;
- Checklist:
- Anesthesia: - request GEA if compartment syn is possible;
- Cardiology
- Blood (4 units)
- X-rays and Template
- Consent
- ATB (High dose Vanc if pt has been in SICU)
- Posting
- Implant Selection;
- Positioning
- Table type and Flouro
- Incision
- Sulcatrans / Cell Saver
- Bone Graft
- Initial Orders: (Post Op Orders)
- NPO p Midnight x Meds
- IVF D5W 1/2 NS c 20 KCL at 100 ml/hr
- 2 large bore IV;
- Foley
- Type & Cross 2-4 units pRBC and/or FFP
- Meds
- Insulin (1/2 NPH dose) + S.S. - Accu Check in AM and on call
- ATB:
- Heparin 5000 units SQ q8 hrs;
- Zantac
- Morphine
- PreOp Labs:
- Musculoskeletal Labs:
- EKG
- CXR
- Urinalysis
- Buck's Traction
- Egg Crate / Pillow and turn 20 deg q2hr;
- Hiboclens Shower and Bactroban to nares q12 hrs until OR
- Cleocin solution 300 mg per 100 ml NS q6hr as mouth wash;
- Physical Exam:
- extent of soft tissue injury
- r/o open pelvic fracture (Gyn/Rectal Injuries)
- Neurologic Injury

