Helton Defino, Fabio Galbusera, Hans-Joachim Wilke
HISTORICAL DEVELOPMENT
Pedicle screw fixation represents a landmark in the field of spinal surgery. In view of the biomechanical advantages of pedicular fixation systems, which provide more tridimensional stability to the vertebral segment with a small area of instrumentation, even in the absence of posterior vertebral elements, and improves outcomes of spinal fusion, this modality of vertebral fixation has gained increasingly widespread acceptance.1-3 The success of the spinal fixation depends on the primary stability and long term stability. Primary stability is related to the spinal fixation system and the long-term stability depends also on the conditions of the treated spinal segment, such as possible osteoporosis.
Pedicle screw fixation is currently one of the most used modalities for internal thoracic and lumbar spine stabilization. Although segmental fixation with wires, bands and hooks still plays a significant role, the biomechanical advantages of the pedicle screw led to an increase of the use of pedicle screw fixation over time. Besides, pedicle screws provide superior clinical results compared to other methods of spine instrumentation. However, in osteoporotic bones “in vitro” similar primary and long-term stability was observed between pedicle screws and a laminar hook system additionally fixed on the lamina with a perforating screw as well as cortical screws were shown to have equivalent pullout strength in osteoporotic bone compared to pedicle screws.4-7
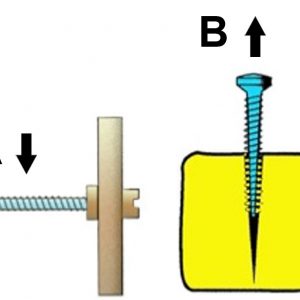
The use of pedicle screw for spinal fixation began in France in 1963 with Roy-Camille, who waited until 1970 to report the technique.8 He promoted the use of pedicle screws as a point of fixation for thoracolumbar segmental fixation. The technique was first applied to treat fractures and later extended to treat tumors, spondylolisthesis and malunions. The earlier version of pedicle screw was monoaxial and coupled with plates; later, it has evolved to the current rod-based system coupled with polyaxial screws (Fig. 9-1).
Although pedicle screw fixation has acceptance in Europe and other countries, there was a controversy in United States regarding its use. The controversy was predominantly due to FDA (Food and Drug Administration) concerns about the safety and effectiveness of the pedicular screw fixation.1 The reason was based only on legal issues, since the American spine societies were in favor of pedicle screw.1 Despite the FDA restriction, American spine surgeons have started to implant pedicle screws in the spine as “off-label” use. The “FDA Classification Panel Meeting for Thoracolumbosacral Pedicle Screw System” started in 1993.
As Europe was the birth place of the pedicle screw, the preliminary evolution of pedicle screw fixation happened there. The Roy-Camille implant was modified to be used in the lumbosacral junction, and an increase in the fusion rate was observed.9-10 Fritz Magerl from Switzerland introduced the concept of angle-stable pedicular fixation that allowed the short stabilization for fractures of the thoracolumbar spine.10 This concept led to the development of the first generation of internal fixators as proposed by Dick, Olerud and Kluger. In the United States, pedicle screws were first used by Harrington to reduce and stabilize high-grade spondylolisthesis,11,12 and Steffee used screws coupled with plates for reduction and stabilization of degenerative spondylolisthesis.13
BIOMECHANICS
Pedicle screw fixation was designed to provide immediate stability, rigid immobilization and short fixation without sacrificing additional motion segments required by other forms of fixation. Knowledge of biomechanics offers the opportunity to predict and avoid surgical constructs that may lead to hardware failure and poor clinical outcomes.
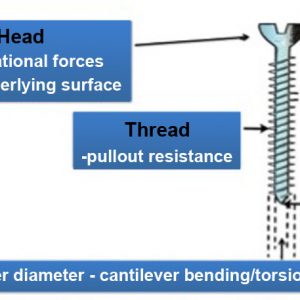
Vertebral fixation system comprises anchorage components (screws, hooks, wires and cables), longitudinal components (rods, plates), transversal connectors and accessories (staples). Pedicle screws are penetrating implants that provide bending and pullout resistance (Fig. 9-2).14
The screw’s bending resistance mostly depends on the screw features itself, such as its material and core diameter. The screw pullout strength depends on other screw features such as the thread and diameter, as well as on the bone around the screw and the preparation of the pilot hole. Failure of pedicle screw can occur at the bone-implant interface (pullout from the bone) or within the instrumentation itself (screw breakage).
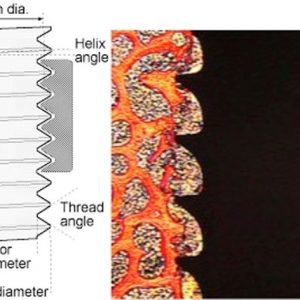
Pedicle screws consist of a head, body and tip, and each part of the screw has a biomechanical importance (Fig. 9-3). The body of the screw has an outer (major) diameter and an inner (minor) diameter.15 The inner core of the screw can be cylindrical or conical. Dual core screws have a thicker diameter around the neck to improve load-bearing capacity.16,17
The screw thread is a ridge wrapped around the core of the screw, which can be cylindrical or conical. The thread depth is the difference between the external and internal diameter of the screw. The distance between the crests of two adjacent threads is called pitch of the thread. The outer diameter of the screw and the thread depth are related to the thread, and they play an important role in screw pullout resistance.14,15,17 The outer diameter of the screw is one of the most important design-related factors for screw pullout resistance.15 However, thread pitch, thread depth and thread shape also influence the pullout resistance. Thread depth, pitch and shape are directly related to the volume of bone inside the thread, and the screw pullout resistance is proportional to the volume of bone between the threads (Fig. 9-4).14,15
The lead is the distance advanced with one revolution. Double lead and dual thread pedicle screws were designed to allow faster insertion. These screws provide a higher insertional torque; however, an improvement in the pullout strength has not been proven yet.18,19 Screw pullout resistance is complex and related to different factors; such as opposite cortical screw purchase,20 screw trajectory, depth of screw penetration21 and screw triangulation,22 tapping, pilot hole preparation, screw reinsertion and bone mineral density. It was experimentally observed that pullout strength of transpedicular thoracic pedicle screws were superior to extrapedicular screws. However, the difference was small and extrapedicular thoracic screws can be an alternative in case of anatomical difficulties.23
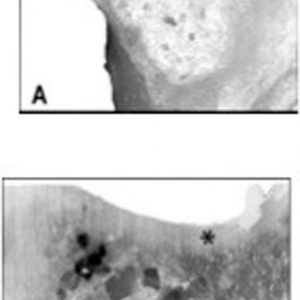
The vertebral pedicle is classically considered to be a cylindrical structure of cortical bone filled with a small amount of cancellous bone. However, this classical description does not correspond to reality, since transverse sections show that the pedicle are tear drop or kidney shaped and contain a small amount of cortical bone and abundant cancellous bone (Fig. 9-5). Pedicle screws do not gain purchase in cortical bone within the pedicle, and alterations in the outer diameter of the pedicle were observed after the introduction of implants of a wider diameter than the diameter of cancellous bone.24 Cortical bone of the vertebral pedicle does not participate to an important extent in the fixation of implants placed inside the vertebral pedicle.25
The depth of pedicle screw insertion is important for screw pullout resistance. However, the increase in pullout strength should be weighted against the risk of increased insertion depth and the potential risks through the anterior cortex rupture. It seems that 80% pedicle screw insertion depth provides a safe and sufficient screw pullout resistance; indeed, 80% penetration depth is 32.5% stronger than 50% penetration.21 Furthermore, the pedicle is more important in resisting pullout than the vertebral body itself (60% versus 40%).26
The trajectory of the pedicle screw also has an influence on the screw pullout resistance. A straightforward screw trajectory has a beneficial effect on the pullout resistance5 as well as the screw convergence. Convergence of pedicle screws by 30° in the coronal plane can increase pullout strength by 28.6%.15,27
The holding power of the pedicle screw is significantly influenced by the size and technique of the pilot hole.28-31 Diameter of the pilot hole in relation to the screw core diameter influences screw-bone contact, insertion torque and pullout strength. In a experiment using sheep, a pilot hole smaller than the internal diameter of the screw promoted greater bone-implant contact and increased area of bone inside the thread of the screw both immediately and after 8 weeks after screw insertion.32
Pilot hole tapping is desirable to achieve correct screw trajectory and also allows checking the pedicle walls before screw insertion. However, tapping weakens the implant-bone interface in cancellous bone and might thus decrease the pullout strength.33 Undertapping by 1 mm is safe and provides the same pullout strength as an untapped screw.19,28,34 Same-size tapping is not recommended as it reduces the screw purchase and its pullout resistance.19
Insertion, back-out and reinsertion of pedicle screws results in reduction of insertional torque and pullout strength.35 The reduction of insertional torque and pullout strength after insertion, back-out and reinsertion was observed in cylindrical and dual-core pedicle screws.36
The mechanical stability of the fixation system relies on the performance of pedicle screws for anchorage into the bone, which, in turn, is directly related to the purchase of the screw into the vertebrae.31,37 As the surgeon cannot change the bone quality, efforts are made to improve the implant design and insertion techniques to achieve better screw fixation.36
OSTEOPOROSIS
An increasing proportion of elderly patients undergo surgical treatment for spinal disorders, and pedicle screw instrumentation is one of the most used systems.38 In osteoporotic bone, screw pedicle fixation can be challenging, because the mechanical stability of the pedicle screw is negatively affected by the low bone mineral density.26,39 An adequate purchase with standard pedicle screw fixation remains a challenge in a spine with poor bone quality. Loosening, migration or back-out of the screw can occur due to poor bone-screw contact.40-43 Strategies have been proposed to enhance the screw anchoring strength in osteoporotic bones such as new screw designs, augmentation techniques,44-46 coatings,47-50 and cortical screws. Biphosphonate treatment and expandable screws have also been used to improve the holding power of the screws by acting on the screw-bone interface and increasing the contact and volume of bone surrounding the screw thread.40,51,52 The anchoring strength in osteoporotic bone can also be improved by using screws that have a conical core with a smaller core at the end, called dual core screws.
Pedicle screws have been augmented with polymethylmetacrilate, calcium ceramics, butyl-2-cyanoacrilate or other materials to improve the strength of bone-screw-interface in osteoporotic bone.51,53 Augmentation can be performed by means of the injection of the material inside the pedicle before screw insertion or through fenestrated or cannulated screws. It was shown that the latter techniques induce higher pullout and fatigue strength than the prefilled technique.52 Fenestrated and cannulated screws allow for a wider distribution of the cement closer to the pedicle leading to greater fixation strength. However, a ten-fold increase of cardiovascular complications with cement augmentation of the pedicle due to cement leakage have been reported, and it was claimed that fenestrated screws might present with a higher risk of screw breakage.51,52,54
The pullout strength of screw augmented with calcium sulfate or PMMA increased by 167% and 199% respectively, compared to unaugmented screws.
Expandable pedicle screws have also been developed to increase the screw-bone interface in osteoporotic bone. In osteoporotic bone, expandable screws have approximately 50% higher pullout strength compared to regular screws, due to better screw-bone-contact promoted by radial expansion at the screw tip diameter. 44,51,53,55,56
Indications
The pedicle is the strongest site accessible through a posterior approach to perform a three dimensional rigid fixation of the vertebra using pedicle screws. Transpedicular screw fixation provides a high mechanical stability, allows correction maneuvers, does not require external immobilization, and it has been used in the surgical treatment of a variety of spinal diseases such as spinal fractures, tumors, infection, spondylolisthesis, scoliosis, lumbar arthrodesis, kyphosis, etc.1
The first use of pedicle screws was in the treatment of thoracolumbar fractures. The possibility of a short, rigid stabilization overcame the disadvantages of distraction-type implants like Harrington rods, which necessitate the inclusion of two or three segments above and below the injured vertebra. In later years, various fixation systems were developed using pedicle screws for fracture treatment. The indication was spread to thoracic fractures as well, and now there is a tendency to perform a percutaneous insertion of the pedicle screws in order to reduce the morbidity of the open access. The pedicle screw fixation devices allow the fusion of fewer motion segments in the treatment of spinal fractures compared to non-pedicular fixation system.1,57
Pedicle screw fixation system has been currently used in the surgical treatment of spinal deformities. Initially pedicle screws were used only in the bottom of the instrumented area in the lumbar spine. As the insertion of the pedicle screw turned out to be safe, screws were applied also in the thoracic spine, and an evolution in the concept of fixations system was observed in this field. The systems for deformity correction have incorporated the pedicle screw in the treatment concept, and the derotation concept was introduced. Pedicle screws are being used in the surgical treatment of different modalities of spinal deformities such as scoliosis, kyphosis, osteotomies and vertebral resection.57
Pedicle screws were a landmark in spinal deformity correction, because they engage in the strongest part of the vertebra and improves the bone-screw interface, thus allowing the application of higher corrective forces to translate, derotate or to perform other maneuvers to correct the deformed spine. Initially only monoaxial screws were used, and, although they showed superiority for vertebral rotation correction, the difficulty aligning the screw and seating the rod into the screw head saddle was a disadvantage. Polyaxial screws provided more freedom as they facilitate the rod insertion into the screw saddle head. However, some polyaxial screw heads can be blocked so that the screw can mimic a monoaxial axial screw for the derotation maneuver.58,59
A more recent application of pedicle screws was the concept of dynamic fixation systems, which are designed to reduce spinal instability while preserving a certain degree of mobility.60
Accuracy of the Implantation
Although pedicle screws have increased in popularity over the last decades and their indications are growing, the accuracy of pedicle screw placement is a critical issue, because there is still a significant number of screw misplacements even in experienced hands.61,62 Screw misplacement can cause a variety of problems to patients with minor to major consequences (radicular pain, weakness or sensory loss, paralysis, major vascular lesion), with lower risks when surgery is performed by an experienced spinal surgeon.47 Nerve root injuries were observed in about 2% of patients, neurological deficits in about 1.3 to 1.8% and radicular pain in 5% of the patients. Approximately 20% of pedicle screws are misplaced when conventional techniques are used and around 7% when navigation was used. Improved instrumentation as well as novel image-guided and navigation techniques have been developed to improve pedicle screw placement.49,50
Regardless of the technique used, the surgeon should have a comprehensive understanding of the spinal anatomy and of techniques for screw insertion. Preoperative images should be evaluated, and the anatomy of the spinal segment to be operated on should be evaluated in detail.
The placement of pedicle screws should be performed in a step-wise sequence that can be divided into exposure, entry point identification, pilot hole, pedicle wall checking, tapping and screw insertion.
The first important component of successful pedicle screw placement is a meticulous exposure of the posterior elements so that the anatomical landmarks can be identified. The spine should be exposed bilaterally to the tips of transverse process and to the lateral border of the superior articular process. The facet joints must be exposed and cleaned of soft tissues. In the thoracic spine, the inferior face is removed for better visualization and identification of the entry point.
The entry point for each pedicle varies according to the spinal level. The entry point in the thoracic spine (T1-T12) is at the junction of the bisected transverse process and lamina at the lateral border of the pars. The starting point above the midthoracic region tends to move slightly lateral and caudal, and it tends to be most medially proximally located at the apical midthoracic spine (T7-T9). The optimal starting point for thoracic pedicle screws based on morphological finding should be 2-3mm lateral to the superior articular facet midline, allowing screw placement in the center of the pedicle. However, the direction of the pilot hole perforation in the axial plane should be considered.63-65
In the lumbar spine, the starting point is at the junction of a vertical line running along the lateral aspect of the facet joint (or the lateral border of the pars articularis) and a line drawn horizontally through the middle of the transverse process. In the upper sacral pedicle the entry point is the intersection of the sacral ala and the inferior margin of the adjacent joint.
The entry point can be marked using an awl or a burr to create a posterior cortical breach and visualization of the cancellous bone of the pedicle.
The pilot hole can be created using a drill, gearshift, probe or dynamic surgical guidance. The direction of the pilot hole should be parallel to the superior endplate of the vertebral body or follow the anatomical axis of the pedicle at thoracic spine in the sagittal plane. In the coronal plane, the pilot hole angulation varies depending on the level. At L1 level, the direction is 10-15 degrees with respect to the horizontal line, and it increases by approximately 5 degrees at the subsequent lower levels.
The next step is to use a ball-tipped probe to check the walls of the pedicle and verify violation or perforation of the pedicle wall. The length of the pilot hole is then measured for an appropriate selection of the pedicle screw length. An optimal screw length should place the tip of the screw about 80% across the vertebral body. The pilot hole can be tapped, again sounded with the ball-tipped probe to check the pedicle walls and finally the appropriate screw can be inserted.
Fluoroscopy-Assisted Techniques
Several techniques have been developed to assist the surgeon in the percutaneous implantation of pedicle screws. If no assistance is used, the surgeon needs to rely on her/his anatomy knowledge and spatial orientation. Little or no operative imaging is used and the accuracy of screw placement depends on the individual experience and skill. The accuracy of pedicle screws inserted by freehand technique has been reported as 5.8% rate of pedicle breaches.47,48,66
Alternatively, fluoroscopically assisted techniques can be used. Compared to the freehand technique, it results in better accuracy by providing a real-time imaging during entry point localization, pilot hole perforation and screw insertion. Fluoroscopy can be used in anteroposterior (AP), lateral or both views. Its use is optional for open screw placement, but it is mandatory for percutaneous techniques. For the latter technique, the C-arm has to be used in both AP and lateral positions; thus the use of two C-arms makes the procedure faster, safer and reduces the amount of radiation.67 The use of fluoroscopy does have some drawbacks such like radiation exposure and the inability to show the spine segment tridimensionally. It displays only two planes and AP view can be difficult to interpret.68
Percutaneous Screw Implantation
Techniques for percutaneous pedicle screw insertion have been developed to allow the placement of the screw with limited exposure of the spine. The percutaneous technique involves the pedicle localization using a Jamshidi needle or K-wire through a stab skin incision.
The first step of the percutaneous technique assisted by fluoroscopy is the positioning of the patient so that the target vertebra can be well centered and visualized on both planes (coronal and sagittal). The entry point is confirmed on a true AP view and a K-wire is used to localize the lateral border and the transverse diameter of the pedicle of the target vertebra. A skin incision 1-2 cm lateral to the skin mark is performed; the fascia and muscle are incised and dissected bluntly until the transverse process is palpated. The Jamshidi needle or K-wire is docked at the starting point (3 o’clock positon for right pedicle and 9 o’clock position for left pedicle). After checking the craniocaudal direction the needle is inserted until the tip is just inside the medial outline of the pedicle on AP view. At this point, a lateral real view is taken, and the needle should be located just before the posterior vertebral border. The needle is then advanced 3-4 mm through the posterior wall of the vertebral body and the lateral view is made to verify the final position. After obtaining a satisfactory positioning of Jamishidi needle, a K-wire is introduced through the core of the needle to guide tapping and screw introduction into the pedicle.69,70
PEDICLE SCREWS FOR DEFORMITY CORRECTION
The use of pedicle screws in the treatment of spinal deformities has allowed greater correction of the curves compared with constructs using hooks, sublaminar wires or hybrids constructs.71 It is believed that the benefit is due to the strong anchorage provided by pedicle screws, which seems to be more important than the used reduction technique. The correction of spinal deformities occurs mainly in the coronal and axial plane; however, correction of hypokyphosis as well as decrease in thoracic kyphosis has been reported.72,73
Pedicle screws provide a greater potential with respect to other anchoring implants for three-dimensional correction of spinal deformities, especially in the transverse plane. Monoaxial screws provided better corrections in the coronal plane than polyaxial screws, as well as efficacy of the derotation technique. However, the use of polyaxial screws is associated with better restoration of the sagittal profile.54,74 Besides, monoplanar screws were developed to improve the ease of rod engagement without reducing the strength in the sagittal plane.75
REFERENCES
- Boos N, Webb JK. Pedicle screw fixation in spinal disorders: a European view. Eur Spine J. 1997;6(1):2-18.
- Farshad M, Farshad-Amacker NA, Bachmann E, Snedeker JG, Schmid SL. Biomechanical comparison of sagittal-parallel versus non-parallel pedicle screw placement. Acta Neurochir (Wien). 2014;156(11):2147-2151.
- Kabins MB, Weinstein JN. The history of vertebral screw and pedicle screw fixation. Iowa Orthop J. 1991;11:127-135.
- An HS, Singh K, Vaccaro AR, et al. Biomechanical evaluation of contemporary posterior spinal internal fixation configurations in an unstable burst-fracture calf spine model: special references of hook configurations and pedicle screws. Spine (Phila Pa 1976). 2004;29(3):257-262.
- Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29(18):2040-2048.
- Korovessis P, Baikousis A, Zacharatos S, Petsinis G, Koureas G, Iliopoulos P. Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (L2-L4) burst fractures. Spine (Phila Pa 1976). 2006;31(8):859-868.
- Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine (Phila Pa 1976). 2000;25:1157-1170.
- Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;(203):7-17.
- Louis R. Fusion of the lumbar and sacral spine by internal fixation with screw plates. Clin Orthop Relat Res. 1986;(203):18-33.
- Magerl F. External skeletal fixation of the lower thoracic and the lumbar spine. In: Uhthoff HK, Stahl E (eds). Current Concepts of External Fixation of Fractures. Berlin, Heidelberg: Springer; 1982. pp. 353-366.
- Harrington PR, Tullos HS. Reduction of severe spondylolisthesis in children. South Med J. 1969;62(1):1-7.
- Harrington PR, Dickson JH. Spinal instrumentation in the treatment of severe progressive spondylolisthesis. Clin Orthop Relat Res. 1976;(117):157-163.
- Steffee AD, Biscup RS, Sitkowski DJ. Segmental spine plates with pedicle screw fixation. A new internal fixation device for disorders of the lumbar and thoracolumbar spine. Clin Orthop Relat Res. 1986;(203):45-53.
- Benzel E. Biomechanics of Spinal Stabilization. 3rd ed. New York: Thieme; 2001.
- Crawford C III, O’Shaughnessy BA, Kuklo TR. Basic pedicle screw and construct biomechanics. In: Bridwell KH, DeWald RL (eds). The Textbook of Spinal Surgery.vol. 1. Philadelphia: Lippincott; 2011.74-85.
- Law M, Tencer AF, Anderson PA. Caudo-cephalad loading of pedicle screws: mechanisms of loosening and methods of augmentation. Spine (Phila Pa 1976). 1993;18(16):2438-2443.
- Skinner R, Maybee J, Transfeldt E, Venter R, Chalmers W. Experimental pullout testing and comparison of variables in transpedicular screw fixation. A biomechanical study. Spine (Phila Pa 1976). 1990;15(3):195-201.
- Mummaneni PV, Haddock SM, Liebschner MA, Keaveny TM, Rosenberg WS. Biomechanical evaluation of a double-threaded pedicle screw in elderly vertebrae. J Spinal Disord Tech. 2002;15(1):64-68.
- Cho W, Cho SK, Wu C. The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg Br. 2010;92(8):1061-1065.
- Maiman DJ, Pintar FA, Yoganandan N, et al. Pull-out strength of Caspar cervical screws. Neurosurgery. 1992;31(6):1097-1101; discussion 1101.
- Krag MH, Beynnon BD, Pope MH, DeCoster TA. Depth insertion of transpedicular vertebral screws into human vertebrae: effect upon screw-vertebra interface strength. J Spinal Disord. 1988;1(4):287-294.
- Ruland CM, McAfee PC, Warden KE, Cunningham BW. Triangulation of pedicular instrumentation. A biomechanical analysis. Spine (Phila Pa 1976). 1991;16(6 Suppl):S270-276.
- White KK, Oka R, Mahar AT, Lowry A, Garfin SR. Pullout strength of thoracic pedicle screw instrumentation: comparison of the transpedicular and extrapedicular techniques. Spine (Phila Pa 1976). 2006;31(12):E355-358.
- Misenhimer GR, Peek RD, Wiltse LL, Rothman SL, Widell EH Jr. Anatomic analysis
- of pedicle cortical and cancellous diameter as related to screw size. Spine (Phila Pa 1976). 1989;14(4):367-372.
- Defino HL, Vendrame JR. Role of cortical and cancellous bone of the vertebral pedicle in implant fixation. Eur Spine J. 2001;10(4):325-333.
- Hirano T, Hasegawa K, Takahashi HE, et al. Structural characteristics of the pedicle and its role in screw stability. Spine (Phila Pa 1976). 1997; 22(21):2504-2509; discussion 2510.
- Barber JW, Boden SD, Ganey T, Hutton WC. Biomechanical study of lumbar pedicle screws: does convergence affect axial pullout strength? J Spinal Disord. 1998; 11(3):215-220.
- Carmouche JJ, Molinari RW, Gerlinger T, Devine J, Patience T. Effects of pilot hole preparation technique on pedicle screw fixation in different regions of the osteoporotic thoracic and lumbar spine. J Neurosurg Spine. 2005:3(5):364-370.
- Chatzistergos PE, Sapkas G, Kourkoulis SK. The influence of the insertion technique on the pullout force of pedicle screws: an experimental study. Spine (Phila Pa 1976). 2010;35(9):E332-337.
- Daftari TK, Horton WC, Hutton WC. Correlations between screw hole preparation, torque of insertion, and pullout strength for spinal screws. J Spinal Disord. 1994;7(2):139-145.
- Pfeiffer M, Gilbertson LG, Goel VK, et al. Effect of specimen fixation method on pullout tests of pedicle screws. Spine (Phila Pa 1976). 1996:21(9):1037-1044.
- Silva P, Rosa RC, Shimano AC, Defino HL. Effect of pilot hole on biomechanical and in vivo pedicle screw-bone interface. Eur Spine J. 2013;22(8):1829-1836.
- Chapman JR, Harrington RM, Lee KM, Anderson PA, Tencer AF, Kowalski D. Factors affecting the pullout strength of cancellous bone screws. J Biomech Eng. 1996;118(3):391-398.
- Kuklo TR, Potter BK, Polly DW Jr., Lenke LG. Monaxial versus multiaxial thoracic pedicle screws in the correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2005;30(18):2113-2120.
- Defino HL, Rosa RC, Silva P, et al. The effect of repetitive pilot-hole use on the insertion torque and pullout strength of vertebral system screws. Spine (Phila Pa 1976). 2009;34(9):871-876.
- Defino HL, Rosa RC, Silva P, Shimano AC, Albuquerque de Paula FJ, Volpon JB. Mechanical performance of cylindrical and dual-core pedicle screws after repeated insertion. Spine (Phila Pa 1976). 2012;37(14):1187-1191.
- Zhang QH, Tan TS, Chou SM. Effects of bone materials on the screw pull-out
- strength in human spine. Med Eng Phys. 2006;28(8):795-801.
- Gaines RW Jr. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82-A(10):1458-1476.
- Reinhold M, Schwieger K, Goldhahn J, Linke B, Knop C, Blauth M. Influence of screw positioning in a new anterior spine fixator on implant loosening in osteoporotic vertebrae. Spine (Phila Pa 1976). 2006;31(4):406-413.
- Christodoulou E, Chinthakunta S, Reddy D, et al. Axial pullout strength comparison of different screw designs: fenestrated screw, dual outer diameter screw and standard pedicle screw. Scoliosis. 2015;10:15.
- Cook SD, Salkeld SL, Stanley T, Faciane A, Miller SD. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004;4(4):402-408.
- Liu D, Wu ZX, Pan XM, et al. Biomechanical comparison of different techniques in primary spinal surgery in osteoporotic cadaveric lumbar vertebrae: expansive pedicle screw versus polymethylmethacrylate-augmented pedicle screw. Arch Orthop Traum Surg. 2011;131(9):227-232.
- Yazu M, Kin A, Kosaka R, Kinoshita M, Abe M. Efficacy of novel-concept
- pedicle screw fixation augmented with calcium phosphate cement in the osteoporotic spine. J Orthop Sci. 2005;10(1):56-61.
- Santoni BG, Hynes RA, McGilvray KC, et al. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9(5):366-373.
- Soshi S, Shiba R, Kondo H, Murota K. An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine (Phila Pa 1976). 1991;16(11):1335-1341.
- Wittenberg RH, Shea M, Swartz DE, Lee KS, White AA 3rd, Hayes WC. Importance of bone mineral density in instrumented spine fusions. Spine (Phila Pa 1976). 1991;16(6):647-652.
- Aoude AA, Fortin M, Figueiredo R, Jarzem P, Ouellet J, Weber MH. Methods to determine pedicle screw placement accuracy in spine surgery: a systematic review. Eur Spine J. 2015;24(5):990-1004.
- Gelalis ID, Paschos NK, Pakos EE, et al. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2012;21(2):247-255.
- Tian NF, Huang QS, Zhou P, et al. Pedicle screw insertion accuracy with different assisted methods: a systematic review and meta-analysis of comparative studies. Eur Spine J. 2011;20(6):846-859.
- Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976). 2007;32(3):E111-120.
- Wan S, Lei W, Wu Z , Liu D, Gao M, Fu S. Biomechanical and histological evaluation of an expandable pedicle screw in osteoporotic spine in sheep. Eur Spine J. 2010;19(12):2122-2129.
- Kueny RA, Kolb JP, Lehmann W, Püschel K, Morlock MM, Huber G. Influence of the screw augmentation technique and a diameter increase on pedicle screw fixation in the osteoporotic spine: pullout versus fatigue testing. Eur Spine J. 2014; 23(10):2196-2202.
- Becker S, Chavanne A, Spitaler R, Kropik K, Aigner N, Ogon M, Redl H. Assessment of different screw augmentation techniques and screw designs in osteoporotic spines. Eur Spine J. 2008;17(11):1462-1469.
- Wilkes RA, Mackinnon JG, Thomas WG. Neurological deterioration after cement injection into a vertebral body. J Bone Joint Surg Br. 1994;76(1):155.
- Rohmiller MT, Schwalm D, Glattes RC, Elalayli TG, Spengler DM. Evaluation of calcium sulfate paste for augmentation of lumbar pedicle screw pullout strength. Spine J. 2002;2(4):255-260.
- Cook SD, Barbera J, Rubi M, Salkeld SL, Whitecloud TS 3rd. Lumbosacral fixation using expandable pedicle screws. An alternative in reoperation and osteoporosis. Spine J. 2001;1(4):109-114.
- Yuan HA, Garfin SR, Dickman CA, Mardjetko SM. A Historical Cohort Study of Pedicle Screw Fixation in Thoracic, Lumbar, and Sacral Spinal Fusions. Spine (Phila Pa 1976). 1994;19(20 Suppl):2279S-2296S.
- Blondel B, Lafage V, Farcy JP, Schwab F, Bollini G, Jouve JL. Influence of screw type on initial coronal and sagittal radiological correction with hybrid constructs in adolescent idiopathic scoliosis. Correction priorities. Orthop Traumatol Surg Res. 2012;98(8):873-878.
- Clement JL, Chau E, Kimkpe C, Vallade MJ. Restoration of thoracic kyphosis by posterior instrumentation in adolescent idiopathic scoliosis: comparative radiographic analysis of two methods of reduction. Spine (Phila Pa 1976). 2008;33(14):1579-1587.
- Lonner BS, Auerbach JD, Boachie-Adjei O, Shah SA, Hosogane N, Newton PO. Treatment of thoracic scoliosis: are monoaxial thoracic pedicle screws the best form of fixation for correction? Spine (Phila Pa 1976). 2009;34(8):845-851.
- Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine (Phila Pa 1976). 1996;21(11):1320-1324.
- Berlemann U, Heini P, Müller U, Stoupis C, Schwarzenbach O. Reliability of pedicle screw assessment utilizing plain radiographs versus CT reconstruction. Eur Spine J. 1997;6(6):406-410.
- Park JH, Jeon SR, Roh SW, Kim JH, Rhim SC. The safety and accuracy of freehand pedicle screw placement in the subaxial cervical spine: a series of 45 consecutive patients. Spine (Phila Pa 1976). 2014;39(4):280-285.
- Wray S, Mimran R, Vadapalli S, Shetye SS, McGilvray KC, Puttlitz CM. Pedicle screw placement in the lumbar spine: effect of trajectory and screw design on acute biomechanical purchase. J Neurosurg Spine. 2015;22(5):503-510.
- Bodon G, Grimm A, Hirt B, Seifarth H, Barsa P. Applied anatomy of screw placement via the posterior arch of the atlas and anatomy-based refinements of the technique. Eur J Orthop Surg Traumatol. 2016;26(7):793-803.
- Belmont PJ Jr, Klemme WR, Robinson M, Polly DW Jr. Accuracy of thoracic pedicle screws in patients with and without coronal plane spinal deformities. Spine (Phila Pa 1976). 2002;27(14):1558-1566.
- Assaker R, Reyns N, Pertruzon B, Lejeune JP. Image-guided endoscopic spine surgery: Part II: clinical applications. Spine (Phila Pa 1976). 2001;26(15):1711-1718.
- Fan G, Zhao S, He S, Gu X, Guan X. Fluoroscopic radiation exposure to operating room personnel in spinal surgery. J Spinal Disord Tech. 2014;27(8):448.
- Gazzeri R. Percutaneous pedicle screw fixation technique in the thoracic and lumbar spine-tips and tricks. Surg Technol Int. 2016; 28:303-310.
- Mohi Eldin MM, Hassan AS. Percutaneous transpedicular fixation: technical tips and pitfalls of sextant and pathfinder systems. Asian Spine J. 2016;10(1):111-122.
- Dobbs MB, Lenke LG, Kim YJ, Kamath G, Peelle MW, Bridwell KH. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus pedicle screws. Spine (Phila Pa 1976). 2006;31(20):2400-2404
- Kim YJ, Lenke LG, Kim J, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2006;31(3):291-298.
- Asghar J, Samdani AF, Pahys JM, et al. Computed tomography evaluation of rotation correction in adolescent idiopathic scoliosis: a comparison of an all pedicle screw construct versus a hook-rod system. Spine (Phila Pa 1976). 2009;34(8):804-807.
- Blondel B, Lafage V, Schwab F, Farcy JP, Bollini G, Jouve JL. Reciprocal sagittal alignment changes after posterior fusion in the setting of adolescent idiopathic scoliosis. Eur Spine J. 2012, 21(10):1964-1971.