Lawrence G. Lenke and Melvin C. Makhni
INTRODUCTION
Management of rigid spinal deformities is complex, technically demanding, and can be fraught with significant complications. Many spinal deformities can be managed without osteotomies, particularly primary deformities without congenital abnormalities. However, patients with severe and rigid deformities and those with spinal imbalance often require osteotomies to obtain adequate correction.
EVALUATION OF SPINAL DEFORMITY
Initial management of any patient with a spinal deformity should consist of thorough patient evaluation. Several factors must be analyzed, including the magnitude, type, location, etiology and rigidity of the deformity, as well as the presence of other deformities that may be present along the entire spinal column. These are best evaluated with full-length spinal radiographs in order to obtain a comprehensive understanding of global alignment, including pelvic parameters. Biplanar EOS radiographs of the entire skeleton (skull to feet) are preferable, although full-length stitched radiographs can be taken as well if EOS is not obtainable. In addition to standard anteroposterior (AP) and lateral radiographs, side-bending images can provide important information about curve flexibility; supine, hyperextension over a bolster, and supine AP and lateral radiographs can also be used to investigate the rigidity of the curves. These images are of value because standing or supine bending films are dependent both on patient effort and ability to maintain balance, while traction radiographs require external force generation that is often difficult to quantify and reproduce. Rigidity of kyphotic curves can also be assessed with the patient in the prone position. The etiology and rigidity of the deformity must be understood for proper surgical planning. Ankylosed or multiple operated curves are likely far more rigid than primary curves, which usually have sufficient intrinsic flexibility through mobile discs to help avoid the need for osteotomies to obtain adequate realignment. In general, it may be helpful to categorize patients as flexible, stiff or stuck/fused, which correlates with increasing likelihood of requiring osteotomies.
The location of the curve may also influence operative planning and whether deformity exists in one or multiple locations in the cervical, thoracic or lumbar spine. This may help determine the optimal approach, for example, in high thoracic curves that may be difficult to approach anteriorly. More importantly, the patient’s entire radiographic and clinical picture must be assembled to identify the locations generating their symptoms so that all sites of compression, instability and relevant deformity may be addressed. At times patients may present with multilevel deformity, but if the symptoms are generated from focal neural compression, a more focused surgery may be indicated. Curve angularity can also aid in planning of potential osteotomies. The deformity angularity ratio (DAR), defined as the curve magnitude divided by the number of involved vertebral segments, can be assessed preoperatively as well.1 Sharp angular deformities, either in the coronal or sagittal plane, are often rigid and compress neural elements. In general, patients with longer, more gradual curves with DAR less than 10-15 may be suitable for multiple posterior column osteotomies. Those with DAR greater than 15-20, in general, are more likely to require three-column osteotomies for adequate decompression and curve correction, via spinal shortening in order to avoid excessive neural stretch with correction.
SURGICAL PREPARATION
Due to the difficulty and inherent risks of deformity correction, optimization of the patient and the surgical environment is essential. The patient should undergo preoperative screening of nutritional, cardiac and respiratory status and as well as an evaluation by the anesthesia team prior to the day of surgery. A complete set of imaging with full-length radiographs and an advanced imaging workup consisting of computed tomography (CT), magnetic resonance imaging (MRI) or CT myelogram, if unable to obtain an MRI. These images should be reviewed in order to assess for fusion mass from prior surgery or auto-fusion between ankylosed levels, to identify all sites of neural compression and to plan sizes and trajectories of instrumentation. The hospital must have adequate resources to manage the patient perioperatively, including intensive care and electrophysiologists for neuromonitoring. These teams, as well as the surgery, nursing and anesthesia teams, should maintain open and frequent communication; maintaining the same teams may help enhance efficiency and work flow, thereby decreasing complications. Routine safety measures should always be adhered to, including chlorhexidine skin preparation, appropriate timing and selection of antibiotics, and perioperative antifibrinolytic use to decrease blood loss unless contraindicated.
SURGICAL APPROACH
Various approaches can be utilized alone or in combination to address rigid spinal deformities. It is necessary to access each site of compression, as well as obtain adequate prophylactic decompression when achieving realignment. Anterior release or discectomy may be beneficial for long, smooth curves, and anterior approach may allow for anterior support and restoration of lordosis, especially in the setting of prior posterior surgeries. However, various situations may increase the difficulty and risks of an anterior procedure. Prior anterior surgery may lead to scarring and increased vascular risk; prior posterior surgery can also cause scarring anteriorly, so it is still important to proceed with caution. High thoracic curves or those with a sharp kyphoscoliosis may be difficult to reach through an anterior-only approach.
While anterior, oblique and lateral approaches can be used, our preferred method is to complete all necessary objectives through a single posterior approach, and for the past seventeen years we have been able to do so with good results. Not only do we feel that optimal results are obtainable from the posterior approach, but we feel optimal correction and safety can be ensured in this manner as well. We prefer a posterior setup on a Jackson frame. The abdomen must remain free to decrease pressure on the venous plexus to reduce bleeding, and the arms, pelvis and chest should be properly padded before the start of the case. Extension bolsters under the thighs for hip extension can facilitate fusion in lordosis; operative frames that allow dynamic bending that compress may also help in achieving further lordosis.
Posterior Column Osteotomy
Overview
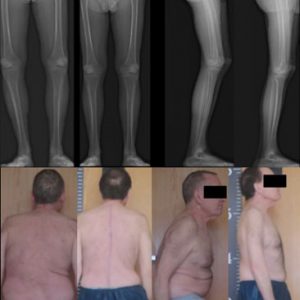
The term posterior column osteotomy encompasses both Ponte and Smith-Petersen Osteotomies (SPOs). These names are often, incorrectly, used interchangeably, so the term PCO was developed to eliminate confusion. Both Ponte and SPOs were developed to achieve lordosis through resection of the posterior column, although SPOs were originally described in ankylosed patients. Due to their immobile discs, they required osteoclasis through the ossified disc and anterior longitudinal ligament (ALL), while Ponte osteotomies rely on mobile discs for correction. Dorward et al. found a mean of 8.8 degrees of coronal correction gained through the use of PCOs in deformity, with more correction obtained in patients under 21 years old or those done in the lumbar or thoracolumbar spine (9.4 and 11.6 degrees, respectively).2 Approximately ten degrees of lordosis is achievable per level with a PCO, but it is quite variable depending on the location of the PCO, with less correction found in the thoracic spine and more in the thoracolumbar (TL) junction and lumbar spine. In general, patients with smooth, gradual multi-level deformity (e.g., Schuermann’s kyphosis) are best suited to benefit from PCOs. However, PCOs can be done at single or multiple levels and can be employed to achieve sagittal or, asymmetrically, to achieve coronal correction as well (Fig. 8-1).
It is important to note that corrections occurring through PCOs are spinal column lengthening procedures. Therefore, it is possible to lose neurologic monitoring data after overcorrection of pre-existing kyphosis using multiple PCOs. If this occurs, the rods should be removed; systemic factors, such as hypotension, should be addressed, and, if no other etiology is found and the neuromonitoring signals return, rods should be reapplied with a lesser degree of correction.
Technique
After meticulous dissection and exposure, the first step in a PCO is resection of the supraspinous and interspinous ligaments. The inferior aspect of the cephalad spinous process and lamina should be removed next, and, if needed for visualization, a portion of the superior aspect of the caudal spinous process and lamina can also be removed. Bilateral inferior articular processes should then be removed with a burr or preferably with an osteotome or rongeur so that bone can be saved for later use as graft. A rent in the ligamentum flavum is created with a rongeur and/or a Woodson elevator, and the plane between the dorsal elements and the dura is defined. A Kerrison rongeur can be used to remove ligamentum flavum and complete the osteotomy through the superior articular facets, resecting on each side from medial to lateral working directly above the superior pedicle pole.
After completion of the resection, posterior compression reduces segmental kyphosis or creates lordosis. The goal after posterior compression is significant central and lateral bone-bone contact, and bone graft should be used as supplement to achieve this, if needed. Because the anterior column remains intact, the goal of PCOs is to compress posteriorly, which, if the patient has mobile disc spaces, causes anterior lengthening. While lengthening occurs in smaller increments than in three-column osteotomies, care must still be taken to not overstretch the cauda or anterior vasculature. The neural elements should also be checked after compressing the osteotomy to ensure that there is no neural impingement. Initial central decompression and complete superior facetectomies will prevent nerve root impingement after osteotomy closure since the pedicles will be closer together and, therefore, the height of the neural foramina decreased.
Pedicle Subtraction Osteotomy (PSO)
Overview
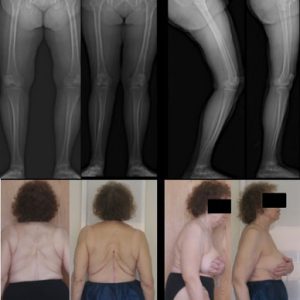
A PSO is performed when a larger amount of correction is needed than can be achieved through a PCO (Fig. 8-2). PSOs are three-column transpedicular wedge resections performed most commonly for patients with fixed sagittal plane imbalance, although they can also be done asymmetrically for patients with coronal plane imbalance as well. This closing wedge osteotomy shortens the spinal canal by compressing the posterior column and maintaining the length of the anterior column (as opposed to PCOs through which the anterior column lengthens in the setting of a mobile disc). It is most often used for fixed imbalance, such as iatrogenic flatback, sharp angular kyphosis or other clinical scenarios that require greater than 30 degrees or 12 cm of angular and sagittal vertical axis correction, respectively. Correction does not rely on mobile disc spaces and, therefore, can be achieved in fused levels; often 30-40 degrees of sagittal correction can be gained with a PSO at a single level. A modification of the PSO, an extended PSO, can also be performed if necessary. Schwab et. al described these as Grade 4 osteotomies; these extended PSOs also include resection of a vertebral endplate and adjacent disc, which may help decrease stretch on the anterior vasculature.3
Better outcomes have been observed when a sagittal vertical axis (SVA) <8 cm is obtained at final follow-up.4 A PSO performed at distal levels could provide larger translational correction proximally as well as greater SVA improvement due to the longer lever arm for correction with a lower correction point. However, Lafage et. al showed little difference between level of PSO and degrees of correction obtained, so other anatomic and radiographic factors should be incorporated in choosing the level of PSO.5 L2 is normally too high unless this is the apex of combined lumbar kyphoscoliosis. L3 is often too high as well and may produce some abdominal protrusion in thinner patients. The apex of lordosis is commonly at L4 or the L4-5 disc, so L4 may be the ideal level for PSO in many patients. Quad weakness may occur after L4 PSO, which can hinder early postoperative rehabilitation, but this is usually transient. A PSO at L5 is beneficial given that L5 has even less nerve roots in the thecal sac, and any neural complication at this level can still leave the patient ambulatory. However, care must be taken at this level anteriorly and laterally given the proximity of the vasculature. For revision cases, the body should not be dissected laterally or anteriorly from posterior, and instead the lateral vertebral body walls should be thinned out interiorly to decrease risks of major vascular complications.
In addition to providing a longer lever arm for correction, L4 or L5 PSOs can improve the pelvic tilt by anteverting the pelvis with posterior closure. If L4 or L5 is chosen, multiple points of sacro-pelvic fixation distally should be considered to support the correction. Six points of fixation, involving two S1 screws and four points of pelvic fixation, allows for good control of the pelvis. Stable fixation is required as well as interbody grafting of proximal and distal disc spaces, as there is an estimated 30% pseudarthrosis rate for PSOs. The use of more than two rods across a PSO has been shown to decrease both rod failure and pseudarthrosis at a minimum 2-year follow-up of these procedures and should be routinely performed.6
Patients must be informed of the risk of complications, including the possibility of neurologic deficit. Recent analysis indicates that up to 22% of patients with complex adult spinal deformity requiring three-column osteotomy may have neurologic impairment at time of discharge, with 11% having a deficit persisting at six months.1 Multiple PCOs should normally be performed rather than a PSO if able to achieve sufficient correction with the former, given that three-column osteotomies have significantly higher blood loss as well as other complications.
Technique
After posterior ligament releases (and removal of any instrumentation if the patient had prior surgery), pedicle screws should be placed in the vertebrae cephalad and caudad to the osteotomy site. The inferior aspect of the cephalad spinous process should be resected as well as the inferior articular facets from the cephalad level. The superior aspect of the posterior elements at the osteotomy level should also be removed. A laminectomy should be performed from mid-pars of the cephalad level to the distal pars of the chosen level. A Kerrison can be used to remove the ligamentum flavum as well as the superior articular facets at the osteotomy level. Extensive central and foraminal decompressions are crucial to avoid neural impingement upon later closure of the osteotomy. It is important to ensure that bone removal is symmetric to avoid coronal plane derangements on closure unless indicated for multiplanar curve correction. Due to the destabilizing nature of all three columns, a temporary rod should be used on one side while working on the contralateral side.
Once the posterior resections are complete, the cancellous bone within the pedicles is removed. Curettes are used to enter the remaining pedicle channel and resect cancellous vertebral body. The medial border of the pedicle is left in place to avoid medial canal perforation during these steps as it acts to hold the exiting root out of the workspace. Care should also be taken medially to protect the exiting nerve roots as they travel infero-laterally past the pedicles. The bone within the vertebral body can be removed in this manner until a triangular wedge of bone has been resected. Bone should be removed until the anterior vertebral body cortex is reached, which is left intact to preserve residual stability and uniplanar sagittal correction if desired. After subperiosteal dissection is performed along the lateral vertebral body, a retractor or sponge is inserted (surface) to protect the lateral segmental vessels and the anterior neurovascular structures.
After sufficient vertebral body is removed through the pedicles, the remainder of the pedicles and the lateral vertebral walls are resected. The posterior vertebral cortex can then be pushed anteriorly away from the dura into the cavity created, and the spine can be collapsed into lordosis. Posterior compression is essential to achieve bone on bone healing; hip hyperextension or bed collapse, in conjunction with properly placed bolsters, can help osteotomy closure, and rods can be placed into the screws previously to maintain correction. Alternatively, a hook-rod construct can provide posterior compression forces to close the PSO without stressing the adjacent pedicle screws. Thorough inspection of the neural elements and coordination with the electrophysiologist performing the neuromonitoring is essential at this stage to minimize chance of neurologic compromise.
Vertebral Column Resection (VCR)
Overview
Vertebral column resections are used when insufficient correction can be achieved by other osteotomies or releases. These powerful osteotomies can be done from a posterior-only approach to achieve significant multiplanar correction, and they have been shown to have improved SRS and ODI outcome score results at five years postoperatively.7,9 However, they are fraught with a 40% overall complication rate even in experienced hands, with up to 22% of patients sustaining initial neurologic deficit.1,8
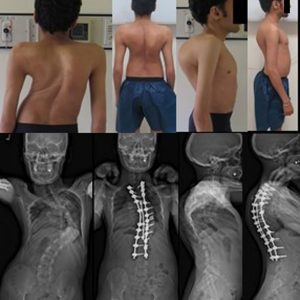
Appropriate indications for VCRs are rigid deformities in patients with severe imbalance and/or neurologic compromise (Fig. 8-3). These deformities may be from congenital kyphosis or hemivertebra, as well as sequelae from prior fusion. Short segment severe deformities, such as spondyloptosis or sharp angular kyphosis from infection or tumor, may also necessitate a VCR.
Patients must be fully evaluated to ensure that they are medically able to sustain such a procedure. Their pulmonary, cardiac and nutrition statuses should then be optimized if they are deemed surgically appropriate. It is important again to mention that patients’ flexibility on physical exam and on a battery of radiographs including bending supine, push-prone, and other studies should be studied to ensure that a VCR is absolutely necessary before proceeding to surgery because of the high percentage and severity of complications. Patients who are myelopathic, have angular kyphosis or prior anterior fusion, or those in whom adequate monitoring is not obtainable are at higher risk for neurologic complications.
Technique
Several preparatory steps for a VCR can be undertaken prior to entering the operating room. Preoperative stretching or in-line traction, via halo-gravity, can be initiated for up to six weeks. The team performing the VCR should ideally have worked together and be experienced in performing three-column osteotomies. Frequent communication with electrophysiology and anesthesia teams should be performed to monitor for neurologic complications, avoid intraoperative hypotension especially during correction, and manage sufficient cardiopulmonary reserve to allow for potentially significant blood loss. A 3D model of the patient’s spine can also be printed and placed in sterile wrapping to be used intra-operatively as a reference. Navigation, robotic guidance technology, sterile 3D printed templates or intra-op CT can be set up to be used to help with screw trajectory as well. Based on the experience of the team and amount of work involved, the decision should be made whether the case should be performed in one sitting or staged. The experience of the senior author suggests that an all-posterior approach is the optimal approach allowing for complete access and control of both the spinal column and neural elements.
After careful soft tissue dissection, a PCO should be performed above and below the level of the VCR unless a severely angular deformity is being treated. Pedicle screws can then be placed at three levels above and below, with no screws at the chosen level. The posterior elements of the vertebrae including the spinous process, laminae, facets and pedicles are removed, ensuring wide central and foraminal decompressions. In the thoracic spine, costotransversectomies are performed bilaterally to remove the medial 5 cm of rib at the apex while protecting the underlying pleura; one exiting nerve root, typically on the convexity of a coronal plane or combined coronal and sagittal plane deformity, is sacrificed in the thoracic spine for additional exposure and to facilitate cage placement.
A temporary rod is placed on the convex side so that most of the initial work can be done from the concave side as the cord will be tented against the concave side and free up the cord and decrease the kinking of the neural elements. This must be done very carefully and with minimal cord retraction but always with dural protection from the high-speed burr that is needed to remove the cortical concave pedicle. As bone is resected from the concave side, the cord will drift in that direction, providing more exposure on the convex side. The vertebral body is then removed from the convex side within the pedicle tracts, with the walls left intact until the body is fully decancellated. The rod can be moved to the other side to complete bilateral resections. The endplates are resected and cephalad and caudal discs removed. The posterior vertebral cortex is pushed anteriorly off the thecal sac, and the anterior wall is thinned down while protecting the anterior vasculature. After completion of the resection, a second temporary rod can be inserted, and the deformity can begin to be corrected. The convex side should always be shortened and then the concave side elongated in several small iterations in order to avoid overstretching the cord.
After appropriate correction, an interbody cage can be inserted as well as final instrumentation. The exposed dural sac can be covered with fibrin glue and bivalved struts of rib, which can protect the cord as well as provide bone graft for osseous fusion. Additional rods should be considered to provide additional stability across the VCR. The use of 3-5 rods may have contributed to patients having no rod fractures as opposed to those with only two rods, in which 20% had rod fractures and 75% of these patients with rod fractures returned to the operating room.6 However, theoretically, the addition of rods may be delaying rather than preventing rod fracture if bony union does not occur, so long-term studies will be needed to reveal the longevity of multi-rod constructs.
NEUROMONITORING FOR OSTEOTOMIES
Due to the high risk of complications from these osteotomies, patients should have appropriate neuromonitoring during these procedures. Several studies have analyzed the efficacy of monitoring in patients undergoing osteotomies and suggest the importance of motor evoked potentials (MEPs) in calling attention to potential neurologic injuries.10-12
One retrospective study reported 37 three-column osteotomies, describing successful responses to monitoring changes.10 Over half of the 23 cases of monitoring changes improved with increasing blood pressure, including all of those that had signal changes before decompression and osteotomy. Of those that did not, two out of three improved simply with osteotomy closure and decrease stretch on the spinal cord, and the remainder improved with further manipulation such as decompression, cage realignment, further decompression and osteotomy closure with less correction. From these data, the authors proposed an algorithm for managing monitoring changes that occur during or after osteotomy. Upon encountering changes, they suggest the first intervention should be increasing blood pressure; steroids can also be considered as a potential adjunct in these settings. If change occurs during bony resection and fails to resolve with systemic treatments, mechanical stretching of the spinal cord should be alleviated. A stabilizing rod can first be inserted and traction released or, if this still does not resolve signals, the osteotomy can be completed and closed. If the signal changes still fail to improve, the osteotomy should be reopened. Closure can be reattempted with less compression and correction to alleviate any excessive cord shortening that may have occurred, and the cage position and extent of decompression can be confirmed as well.
CONCLUSION
Due to the increasing risk for complications with larger corrective osteotomies, effort should be taken to fully evaluate the deformity and consider the minimal operative intervention required to achieve the surgical goals. This should be done through a shared decision model with the patient after disclosure of the spectrum of potential complications that could arise from the surgery.
SUGGESTED READINGS
- Wang XB, Lenke LG, Thuet E, Blanke K, Koester LA, Roth M. Deformity angular ratio describes the severity of spinal deformity and predicts the risk of neurologic deficit in posterior vertebral column resection surgery. Spine (Phila Pa 1976). 2016;41(18):1447-1455.
- Lenke LG, Sides BA, Koester LA, Hensley M, Blanke KM. Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res. 2010;468(3):687-699.
REFERENCES
- Lenke LG, Fehlings MG, Shaffrey CI, et al. Neurologic outcomes of complex adult spinal deformity surgery: results of the prospective, multicenter Scoli-RISK-1 Study. Spine (Phila Pa 1976). 2016;41(3):204-212.
- Dorward IG, Lenke LG, Stoker GE, Cho W, Koester LA, Sides BA. Radiographic and clinical outcomes of posterior column osteotomies in spinal deformity correction. Spine (Phila Pa 1976). 2014;39(11):870-880.
- Schwab F, Blondel B, Chay E, et al. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2014;74(1):112-120.
- Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine (Phila Pa 1976). 2007;32(20):2189-2197.
- Lafage V, Schwab F, Vira S, et al. Does vertebral level of pedicle subtraction osteotomy correlate with degree of spinopelvic parameter correction? J Neurosurg Spine. 2011;14(2):184-191.
- Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM. Comparison of standard 2-rod to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976). 2014;39(22):1899-1904.
- Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH. Posterior vertebral column resection for severe spinal deformities. Spine (Phila Pa 1976). 2002;27(21):2374-2382.
- Lenke LG, O’Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke KM. Posterior vertebral column resection for severe pediatric deformity: minimum two-year follow-up of thirty-five consecutive patients. Spine (Phila Pa 1976). 2009;34(20):2213-2221.
- O’Neill KR, Lenke LG, Bridwell KH, et al. Clinical and radiographic outcomes after 3-column osteotomies with 5-year follow-up. Spine (Phila Pa 1976). 2014;39(5):424-432.
- Jarvis JG, Strantzas S, Lipkus M, et al. Responding to neuromonitoring changes in 3-column posterior spinal osteotomies for rigid pediatric spinal deformities. Spine (Phila Pa 1976). 2013;38(8):E493-503.
- Lieberman JA, Lyon R, Feiner J, Hu SS, Berven SH. The efficacy of motor evoked potentials in fixed sagittal imbalance deformity correction surgery. Spine (Phila Pa 1976). 2008;33(13):E414-424.
- Cheh G, Lenke LG, Padberg AM, et al. Loss of spinal cord monitoring signals in children during thoracic kyphosis correction with spinal osteotomy. Spine (Phila Pa 1976). 2008;33(10):1093-1099.