Brian J. Neuman and Khaled Kebaish
INTRODUCTION
The development of a pseudarthrosis at lumbosacral junction continues to be a concern in spine surgery. Fixation failure due to poor bone quality of the sacrum and substantial biomechanical forces at this junction leads to a cascade of events that result in a pseudarthrosis. Historically, nonunion rates have been reported as high as 50%. 1,2 The development of sacropelvic fixation techniques has lessened the risk of implant loosening at the lumbosacral junction, limiting motion in this area thus allowing adequate time for the fusion to develop. The following chapter will review the various methods of sacropelvic fixation as well as discuss the advantages and disadvantages of each method.
INDICATIONS
Numerous indications for sacropelvic fixation exist. The main concept to using sacropelvic fixation is to eliminate cantilever forces as well as to diminish a flexion moment at the lumbosacral junction. By providing a distal foundation with pelvic fixation these forces are reduced, decreasing the risk of implant loosening that results in a nonunion.3 In the clinical setting, the indications to apply this method of thought and include sacropelvic fixation is in long fusions to the sacrum, high-grade spondylisthesis, corrective osteotomy in the lumbar spine to correct a flat-back deformity, correction of pelvic obliquity, sacral fractures resulting in spinopelvic dissociation and sacrectomy.
The most common reason for using sacropelvic fixation is long fusions to the sacrum. Long fusions that end at the sacrum without additional anchors into the pelvis have a pseudarthrosis rate as high as 44%.4 Clinically, there is some debate on what constitutes a long fusion to the sacrum that would require sacropelvic fixation. Multiple studies advocate using sacropelvic fixation only when the upper instrumented level (UIV) is at or above the thoracolumbar junction.2,5,6 Others suggest that sacropelvic fixation should be used in any fusion to the sacrum with the UIV being L2 or higher.7,8 A recent biomechanical study demonstrated that the use of sacropelvic fixation protects the sacral screws when the UIV is L3 and above.9 Among surgeons it does appear there is a consensus that any fusion to the sacrum with the UIV being above the thoracolumbar junction requires sacropelvic fixation. There is still some debate, though, if fusions to the sacrum with the UIV in the upper lumbar spine should also require sacropelvic fixation; however, the previous mentioned studies suggest so.
Similar to long fusions to the sacrum, the reduction of a high-grade spondylolisthesis also places high biomechanical stress on the S1 screws, and the placement of pelvic fixation can greatly limit the forces on these screws. 5,10-12
TECHNIQUES OF SACROPELVIC FIXATION
Sacral Alar Screws
Sacral alar screws are directed approximately 30-45 degrees laterally and are placed in the lateral anterior cortical bone of the sacrum known as the ala.13 The placement of these screws has a narrow safe zone where they can be inserted. Failure to adequately place these screws can lead to injury to either the lumbosacral trunk or the internal iliac vein. Not only do these screws have a high risk of injury to vital structures, they also have a high rate of pseudarthrosis in long fusions despite have high pullout strength.4,14 Due to the high complication risk and the development of newer techniques, the sacral alar screws have limited use.
Jackson Intrasacral Rods
Jackson intrasacral rods are vertically inserted in the lateral sacral area to the level of S2 and are attached to the S1 pedicle screws.15 The mechanism behind this method is that the sacroiliac ligaments and the portion of the ilium posterior to these rods provide enough support to limit pull out. The advantage of this method compared to other pelvic fixation methods is it does not cross the sacroiliac joint. However, it has limited use do to being technically demanding and because some patients do not have the sufficient sacrum size to place these rods to allow for adequate fixation. There is also concern that these rods do not have any biomechanical advantage when compared to traditional iliac screws and, therefore, are in limited use.16
Kostuik Transiliac Bar
The Kostuik transiliac bar is passed 1-2 cm anteriorly to the posterior superior iliac spine bilaterally and is attached to the S1screws with a longitudinal rod connecting this fixation to the rest of the construct through connectors (Fig. 9-1).17 This fusion technique has demonstrated a 97% fusion rate at the lumbosacral junction.17 However, it requires multiple additional connectors and is less effective in limiting the flexion/extension motion at the lumbosacral junction than the iliac or the S2AI screws.
Galveston Iliac Rods
Galveston iliac rods are a contoured rod which is tunneled under the paraspinal muscles and is inserted between the inner and outer tables of the ilium.18 The iliac portion of the rod angles 20-25 degrees laterally from the posterior superior iliac spine and about 35 degrees caudally from the vertical. These rods are used mostly to treat neuromuscular scoliosis. Fusion rates with this technique range between 88-94%.4,19,20 The disadvantage of this technique is that the implants can become prominent and also the rod can be difficult to contour to the spine. Also, despite a fusion occurring at the lumbosacral region, a high incidence of implant loosening occurs due to micromotion at the tip of the rod and can lead to the need to remove the rod due to pain.19, 21
Iliac Screw
The modern development of the use of modular implants, pedicle screws, for spine fixation has led to the development of iliac screw fixation. Iliac screw insertion point is at the posterior superior iliac spine (PSIS) and is inserted at an angle of 25 degrees laterally from midline and 30 degrees caudal from the vertical. Offset connectors are typically used to connect the screw to the longitudinal rods (Figure 9-2). Some newer technique methods start the placement of the screw on the medial border of the PSIS or the rod is contoured so an offset connector is not needed. Iliac screw fixation allows one to obtain powerful control of the pelvis and allows extensive purchase of the ilium with using a screw length of 80-100 mm.22 Biomechanical studies have shown that the pullout strength of iliac screws are about 3 times higher than that of the Galveston rods which has shown higher fusion rates with the use of iliac screws.20,23,24 The disadvantage of this technique is these screws pose a risk of substantial morbidity. Due to the entry point of these screws at the PSIS, extensive surgical dissection is needed and may increase the risk of infection. The infection rate associated with iliac screw fixation is reported to be about 4%.24 The other major concern with placement of these screws is instrumentation prominence. Tsuchiya et al. reported a 34% revision rate at 5 years for removal of iliac screws due to prominence.25
S2-Alar-Iliac (S2AI) Fixation
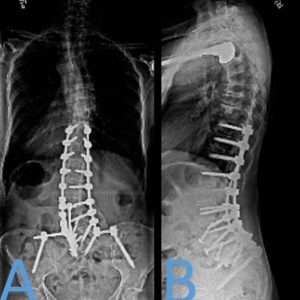
S2AI screws have been developed to provide iliac fixation with a starting point in line with the S1 pedicle screw. The starting point for this screw is the midpoint of a line that connects the lateral edge of the S1 and S2 dorsal foramina. 26 Compared to traditional iliac screws the starting point for the S2AI screws is approximately 15 mm deeper, which lessens screw prominence.27 Other advantages of the S2AI screws is less need of dissection laterally, using only one rod to connect all points of fixation without a need for additional connectors, and it does not interfere with iliac bone graft harvest, which can occur with iliac screws. Biomechanically, the S2AI screws tested equivalent to iliac screws in regards to lessening S1 screw strain.28 The placement of S2AI screws have several advantages over iliac screw placement. With that said, there is a learning curve for placing these screws, and, initially when placing them, it would be best to place them with fluoroscopy guidance. After the starting point, the trajectory is towards the anterior inferior iliac spine, which is lateral, approximately 40 degrees to the horizontal plane, and caudally about 20-30 degrees. The actual degree of caudal angulation relies on the pelvic tilt.29 Assessing the trajectory with fluoroscopy is best done after crossing the SI joint. The anteroposterior view and a teardrop C-arm view is beneficial to show the pelvis and sciatic notch and help guide the initial trajectory and ensure that the screw is in the thickest bone with no cortical breach (Fig. 9-3). A screw length greater than 80 mm and diameter of great than 8 mm is recommended (Fig. 9-4).


CONCLUSIONS
The most common indication to use pelvic fixation is with long fusions to the sacrum. Without this fixation, there is a high rate of pseudarthrosis at the lumbosacral junction, which is mostly due to the high biomechanical stress on this level. Through the years multiple methods for pelvic fixation have been developed but, currently, the Galveston technique, iliac screws and S2AI screws are most popularly used. Each of these current methods has its advantages and disadvantages but is does appear the S2AI screws are most promising in terms of minimizing previous concerns with sacropelvic fixation. With that said, any surgeon performing complex reconstructive spine surgery should be familiar with how to perform all methods of sacropelvic fixation.
PEARLS AND PITFALLS
- Sacropelvic fixation should be used in all long fusions to the sacrum, high-grade spondylolisthesis, corrective osteotomy in the lumbar spine, correction of pelvic obliquity, sacral fractures resulting in spinopelvic dissociation and sacrectomy.
- Various methods of sacropelvic fixation exist with the current techniques being the Galveston technique, iliac screw technique and the S2-Alar-Iliac technique.
- Due to the increased risk of infection and screw prominence with iliac screws, S2AI screws should be considered due to just as favorable results as iliac screws with decreased risk of complications.
- When first leaning to place S2AI screws, it may be beneficial to use fluoroscopy guidance.
SUGGESTED READING
- Allen BL Jr, Ferguson RL. The Galveston experience with L-rid instrumentation for adolescent idiopathic scoliosis. Clin Orthop Relat Res. 1988;229:59-69.
- Andrade NS, Okafor L, Neuman BJ. Novel Technique for Sacral Alar-Iliac(S2AI) Fixation. Clin Spine Surg. 2018;31(9):373-376.
- Chang TL, Sponseller PD, Kebaish KM, Fishman EK. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976). 2009;34(5):436-440.
- Elder BD, Ishida W, Lo SL, et al. Use of S2-alar-iliac screws associated with less complications than iliac screws in adult lumbosacropelvic fixation. Spine (Phila Pa 1976). 2017;42(3):E142-E149.
- Lebwohl NH, Cunningham BW, Dmitriev A, et al. Biomechanical comparison of lumbosacral fixation techniques in a calf model. Spine (Phila Pa 1976). 2002;27:2312-2320.
- Tsuchiya K, Bridwell KH, Kuklo TR, Lenk LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006;31(3):303-308.
REFERENCES
- Thompson WA, Ralston EL. Pseudarthrosis following spine fusion. J Bone Joint Surg Am. 1949;31(A):400-405.
- Devlin VJ, Asher MA. Biomechanics and surgical principles of long fusions to the sacrum. Spine State Art Rev. 1996;10:515-544.
- Alegre GM, Gupta MC, Bay BK, Smith TS, Laubach JE. S1 screw bending moment with posterior spinal instrumentation across the lumbosacral junction after unilateral iliac crest harvest. Spine (Phila Pa 1976). 2001;26(18):1950-1955.
- Devlin VJ, Boachie-Adjei O, Bradford DS, Ogilvie JW, Transfeldt EE. Treatment of adult spinal deformity with fusion to the sacrum using CD instrumentation. J Spinal Disord. 1991;4(1):1-14.
- Bridwell KH, Kuklo T, Edwards CC II, et al. Sacropelvic Fixation. Memphis, TN: Medtronic Sofamor Danek; 2004.
- Perra JH. Techniques of instrumentation in long fusions to the sacrum. Orthop Clin North Am. 1994;25(2):287-299.
- Kostuik JP. Treatment of scoliosis in the adult thoracolumbar spine with special reference to fusion to the sacrum. Orthop Clin North Am. 1988;19(2):371-381.
- Kostuik JP, Errico TJ, Gleason TF. Techniques of internal fixation for degenerative conditions of the lumbar spine. Clin Orthop Relat Res. 1986;(203):219-231.
- Cunningham BW, Sefter JC, Hu N, Kim SW, Bridwell KH, McAfee PC. Biomechanical comparison of iliac screws versus interbody femoral ring allograft on lumbosacral kinematics and sacral screw strain. Spine (Phila Pa 1976). 2010;35(6):E198-205.
- Chewning SJ Jr. Pelvic fixation. Spine State Art Rev. 1992;6:359-368.
- Potter BK, Kuklo TR, O’Brien MF. Sacro-iliac fixation for treatment of high-grade spondylolisthesis. Semin Spine Surg. 2004;16:119-125.
- Molinari RW, Bridwell KH, Lenke LG, Ungacta FF, Riew KD. Complications in the surgical treatment of pediatric high-grade, isthmic dysplastic spondylolisthesis. A comparison of three surgical approaches. Spine (Phila Pa 1976). 1999;24(16):1701-1711.
- Mirkovic S, Abitbol JJ, Steinman J, et al. Anatomic consideration for sacral screw placement. Spine (Phila Pa 1976). 1991;16(6 Suppl):S289-294.
- Zindrick MR, Wiltse LL, Widell EH, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;(203):99-112.
- Jackson RP, McManus AC. The iliac buttress. A computed tomographic study of sacral anatomy. Spine (Phila Pa 1976). 1993;18(10):1318-1328.
- Lebwohl NH, Cunningham BW, Dmitriev A, et al. Biomechanical comparison of lumbosacral fixation techniques in a calf spine model. Spine (Phila Pa 1976). 2002;27 (21):2312-2320.
- Moshirfar A, Rand FF, Sponseller PD, et al. Pelvic fixation in spine surgery. Historical overview, indications, biomechanical relevance, and current techniques. J Bone Joint Surg Am. 2005;87 Suppl 2:89-106.
- Allen BL Jr, Ferguson RL. The Galveston experience with L-rod instrumentation for adolescent idiopathic scoliosis. Clin Orthop Relat Res. 1988;(229):59-69.
- Gau YL, Lonstein JE, Winter RB, Koop S, Denis F. Luque-Galveston procedure for correction and stabilization of neuromuscular scoliosis and pelvic obliquity: a review of 68 patients. J Spinal Disord. 1991;4(4):399-410.
- Saer EH 3rd, Winter RB, Lonstein JE. Long scoliosis fusion to the sacrum in adults with nonparalytic scoliosis. An improved method. Spine (Phila Pa 1976). 1990;15(7):650-653.
- Broom MJ, Banta JV, Renshaw TS. Spinal fusion augmented by Luque-rod segmental instrumentation for neuromuscular scoliosis. J Bone Joint Surg Am. 1989;71(1):32-44.
- Berry JL, Stahurski T, Asher MA. Morphometry of the supra sciatic notch intrailiac implant anchor passage. Spine (Phila Pa 1976). 2001;26(7):E143-148.
- Schwend RM, Sluyters R, Najdzionek J. The pylon concept of pelvic anchorage for spinal instrumentation in the human cadaver. Spine (Phila Pa 1976). 2003;28(6):542-547.
- Kuklo TR, Bridwell KH, Lewis SJ, et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976). 2001;26(18):1976-1983.
- Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006;31(3):303-308.
- O’Brien JR, Yu WD, Bhatnager R, Sponseller P, Kebaish KM. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976). 2009;34(12):E439-442.
- Cheng TL, Sponseller PD, Kebaish KM, Fishman EK. Low profile pelvic fixation: anatomic parameter for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976). 2009;34(5):436-440.
- Sutterlin CE 3rd, Field A, Ferrara LA, Freemna AL, Phan K. Range of motion, sacral screw and rod strain in long posterior spinal constructs: a biomechanical comparison between S2 alar iliac screws with traditional fixation strategies. J Spine Surg. 2016;2(4):266-276.
- Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976). 2010;35(25):2245-2251.