Hanna Hebelka and Helena Brisby
INTRODUCTION
Degenerative spondylolisthesis (DS) is an acquired sagittal translation of one vertebra relative to the subjacent one, without a pars interarticularis defect, caused by degenerative changes.1-3 DS is commonly referred to as an anterolisthesis even though it may also be a retrolisthesis, but to a lesser extent. The most common level for DS is L4-L5 followed by L5-S1, with anterolisthesis being most common at L4-L5 and retrolisthesis more common in L5-S1 and in individuals with reduced lordosis.4-11 This chapter aims to provide the best imaging strategy in obtaining the DS diagnosis. Clinical evaluation, with a thorough physical examination and detailed penetration of symptomatology, is an important step in the diagnosis of DS. The clinical presentation of DS has a wide spectrum ranging from no symptoms at all to back pain with or without radicular symptoms, leg pain, neurogenic claudication, muscle weakness, etc.4-12 Details regarding clinical evaluation of symptomatology are covered in Section 15 Chapter 1 of this publication. When the symptomatology and physical examination points to DS, radiological imaging is then used to confirm the diagnosis and possibly also advise regarding the clinical relevance of the DS in relation to other radiological findings.
RADIOGRAPHS IN THE DIAGNOSIS OF DS
Standard radiographs in anteroposterior (AP) and lateral views in a neutral position are considered the most appropriate imaging test to detect DS.1,13,14 Scoliosis and/or lateral translation are evaluated on AP images while vertebral body height and sagittal translation are best evaluated on the lateral radiographs.2 To achieve mechanical impact, studies recommend that these images be obtained in the standing position,1,12,15-19 since up to 1/3 of DS will be missed on imaging performed in a supine position.16,18,20,21 As an example, Segebarth et al. recently investigated 416 patients with degenerative spine conditions in whom supine MRI and standing radiographs (flexion/extension and lateral) had been performed.18 One hundred nine patients were found to have DS on standing radiographs, however 31 of those were undiagnosed on the supine MRI.18 This highlights the importance of performing weight-bearing imaging investigations when diagnosing and evaluating the grade of DS.
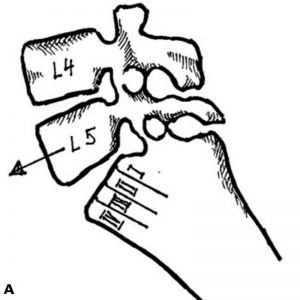
Radiographs are particularly able to demonstrate anterolisthesis of one vertebra relative to the subjacent, without a pars interarticularis defect (Fig. 2-1).14 Examples of concomitant changes that might be detected at radiographs are: disc space narrowing, endplate lesions, osteophytes and facet joint sclerosis.4,5,21,22 In addition, DS is frequently accompanied by degenerative scoliosis, sometimes even with elements of rotational translation, which might be a diagnostic challenge. Regarding alignment, degenerative spinal changes may, in addition to sagittal translation, lead to a kyphotic disc angle at the affected level.23 Sagittally-oriented facet joints are also associated with the presence of DS, though primarily with anterior translation and not posterior translation.11
Malalignment of the spinal processes on lateral radiographs can be seen in DS, due to anterior translation of the entire vertebra, since the neural arch is intact as opposed to in isthmic spondylolysis.5 Oblique AP views, or “scottie dog,” are traditionally used to detect isthmic spondylolisthesis and may reveal a collar on the “dog,” differentiating isthmic spondylolisthesis from DS.2,4,5 However a recent study did not show increased specificity and sensitivity in identifying spondylolysis by adding oblique views as compared with standard views alone.24
MEASURING TECHNIQUES
The magnitude of sagittal translation is often called “slip” and is measured in the lateral view (Fig. 2-2).23,25 Two methods are commonly used to grade spondylolisthesis, irrespective of its type (isthmic or degenerative): the Meyerding Classification26 and the Taillard Method,27 respectively. In the Meyerding Classification, the superior aspect of the inferior vertebra is divided into quartiles on the sagittal view and graded I-IV, representing a slip of the superior vertebra of I, II, III or IV quarters, respectively (Fig. 2-3A). Grade V refers to when one vertebra has slipped off the inferior vertebra entirely, i.e., spondyloptosis.3 According to Taillard, the sagittal translation is classified in percentage of the slip of the superior vertebra relative to the superior aspect of the inferior vertebra (Fig. 2-3B). Due to higher reproducibility, the Taillard Method is favored by most authors.4,5,28 Regarding progression, a slip ≥ 20% is considered relevant, since up to 15% error in intra/inter observer measurements has been reported.5,28,29
INTERVERTEBRAL INSTABILITY
DS is often considered to be associated with pathological vertebral movement, i.e., instability.21,25 This instability theory is based on the occasional findings of increased translation on functional imaging. This theory has also contributed to the popularity of adding fusion surgery in patients with spinal stenosis in need of decompression surgery, aiming to stabilize a DS segment.23,30 A recent randomized controlled trial (RCT) challenges this instability theory by showing no clinical benefit to using fusion as an adjunct to decompression in DS patients.31 The importance of imaging and how to define potential “instability” in DS patients thus needs to be questioned. However, functional imaging is still widely used and the body of literature regarding DS “instability,” and how to best image it, is extensive, which is why this subject will be briefly covered here.
FUNCTIONAL RADIOGRAPHS
The range of segmental vertebral mobility in DS is wide, without any universally accepted definition for either the term “instability” or which imaging techniques should be adopted to verify it – uniform reference standards are lacking.1 Various studies have also reported conflicting results regarding the association between symptoms and DS slip detected with radiology.8,9,21,32,33
To quantify mobility in DS, many doctors employ the use of functional imaging techniques, such as lateral flexion/extension radiographs, since they have the potential to reveal an increased translation.15,34-39 A difference in vertebral slip of ≤ 3 mm between flexion and extension (functional radiographs) has been seen in a majority of asymptomatic subjects.3,40,41 Further, a static translation of > 3 mm, on either extension or flexion radiographs, has been reported in up to 42% in asymptomatic individuals.34 A cut off value of > 3 mm has therefore been accepted by many studies as a sign of abnormal sagittal translation,21,31,42-45 whereas others adopt a change in slip of ≥ 8% or ≥ 4 mm.7,34,46-48
Because of its simplicity, low expense and wide availability, flexion/extension radiographs are the most widely used functional imaging method regarding DS instability.21,38,49-51 Knutsson et al. were one of the first to state that flexion/extension radiographs revealed instability, with many followers also claiming that such functional imaging is important for assessing grade of pathological translation in DS.52 Functional radiographs have in several studies revealed findings not shown on conventional radiographs.6,16,25,44,46,47 For example, Cabraja et al. found what they defined as a pathological slip in 11% of their 100 studied spondylolisthesis patients (83% DS) with flexion/extension radiographs, which had not been apparent in standing/recumbent position radiographs.46 Despite this study’s finding, in most patients, standing radiographs compared with recumbent position radiographs reveal greater sagittal translation compared to flexion/extension radiographs.46 Several others support the use of standing/supine radiographs instead of flexion/extension radiographs.15,16,18,46 Regarding posterior translation, increased incidence has been reported adjacent to discs that are ankylosed or fused. For example, retrolisthesis has been shown postoperatively in 15% of segments cranial to fused disc levels on extension radiographs.53
Various other functional imaging methods have been proposed, such as functional radiographs in seated position and traction/compression radiographs, whereas others claim that flexion/extension in the supine position is preferable to reveal movement in a segment with DS.25,47,48,54,55 The argument for the latter is that pain-induced spasms in the paraspinal muscles are inhibited in supine position and therefore might reveal movement in the segment better than in the standing position.46-48,54,56
It is important to highlight that although functional imaging methods may reveal/increase translation and movement in a spinal segment, this is not synonymous with required changes to clinical decision making. For example, Försth et al. showed in their RCT that despite a sagittal slip over 7 mm on lateral radiographs, there was no difference in clinical outcome comparing decompression combined with fusion with decompression alone.31 A vast majority of doctors today seem to believe that the additional value of functional imaging techniques is limited in the routine clinical situation.15,18,20,21,40,57 Another important reason to question routine use of functional imaging is the non-standardized technique, i.e., lack of routine reference standards and reproducibility.20 Patient positioning relative the X-ray beam, differences in magnifying factor, vertebral tilt and rotation can affect reproducibility with measuring variations up to 10–15%.28,38,50,58 Further arguments for the limited value of functional radiographs is the large variation in the general population and the decreased range of motion of the spine in patients suffering from pain.40,57,59,60
To summarize, considering the limited evidence of its value, cost and radiation, the use of routine functional imaging is not recommended.1,35 Functional imaging should rather be reserved for clinically challenging patients in whom the results of the investigations are likely to affect therapy.15,20,35,36
MAGNETIC RESONANCE IMAGING (MRI) AND DS
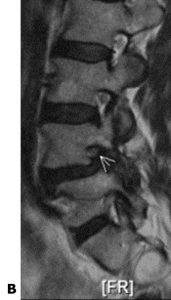
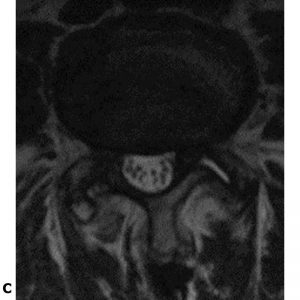
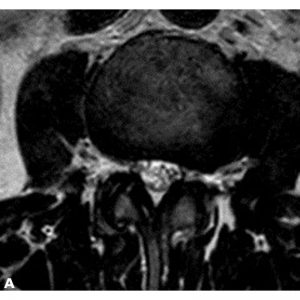
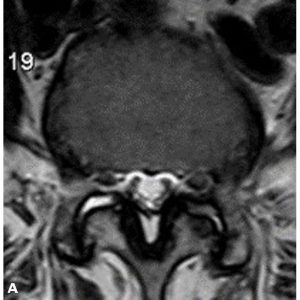
MRI is the most appropriate modality to image spinal canal stenosis or foraminal stenosis accompanying DS.1,2,4,14,22,61 Other MRI findings frequently accompanying DS are facet joint hypertrophy and effusion, synovial cysts, high grade osteoarthritis and thickened ligamentum flavum.1,4,62,63 Spinal MRI should at minimum include conventional sagittal and axial T1 and T2-weighted sequences.2,22 There are no universally accepted quantitative criteria for which MRI parameters that are best for evaluation of spinal stenosis. Examples of various measurements used are cross-sectional dural sac area, AP diameter of the osseous spinal canal, foraminal diameter, lateral recess height and angle and ligamentous interfacet distance.61,64 T1-weighted imaging provides detailed information regarding anatomical structures of foremost soft tissues, and pathology within these, while T2-weighted images are best to visualize the spinal canal and foraminal recesses.3 The cross-sectional dural sac area and AP diameter of the dura are best evaluated at axial T2-weighted images while parasagittal images can display nerve root entrapment by osteophytes, or protruding disc, at the level of the foramina.3 Diminished fat surrounding the root in the foramina is a qualitative parameter indicating foraminal stenosis affecting the nerve root (Fig. 2-4). In 2010, Barz et al. introduced the “positive sedimentation sign,” in which the nerve roots are “floating” within the dural sac as opposed to, due to gravity, being packed together within the posterior aspect of the dura on supine axial MRI images (Fig. 2-5). This sign, the absence of nerve root sedimentation, has been reported to be associated with symptoms of lumbar spinal stenosis.65,66
Facet joint effusion is highly indicative of DS16,62,63,67 and appears to have a linear correlation with the degree of slip.39,42,63,68,69 Facet joint effusion size, best seen on axial T2-weighted images, is measured at the greatest distance between the articular surfaces (Fig. 2-6). According to North American Spine Society’s (NASS) Guidelines 2016, facet joint effusion > 1.5 mm on supine MRI suggests DS and if detected without previous radiographs, standing lateral radiographs are recommended, since DS can be occult/reduced in supine position and facet joint effusion indicate possible movements of the affected segment.1,39,42,62,68
FUNCTIONAL MRI IMAGING
The development of open MRI systems provides new opportunities to image the spine in various positions (standing, sitting, flexion/extension). Both axial loading during MRI (alMRI) and upright MRI have, similar to functional radiographs, been reported to reveal/increase DS slip as compared to in the supine position.12,19,44,70,71 For example, alMRI has been shown to reduce the cross-sectional dural area compared with recumbent MRI without load71,72 and MRI performed in a sitting position can reveal anterolisthesis to a greater extent and in more patients as compared to supine MRI.70 Recently, Splendiani et al. investigated how the change of MRI position, from supine to upright, influenced spinal changes like disc herniations, spinal stenosis, sagittal translation and lumbar lordosis angle in 4305 low back pain patients.44 1178 of these patients had a sagittal translation (> 3 mm) on either supine or upright MRI. Upright MRI revealed significant alterations, defined as the appearance of, or an increase of changes between the positions, in 715 of these 1178 patients. These MRI techniques provide an excellent opportunity to investigate the effect of kinematics on spinal structures, thus having the potential to add clinical useful information for individual DS patients. However, as with functional radiographs, the evidence is insufficient to recommend for or against routine functional MRI.1,21 Rather, alMRI or upright MRI should only be used in selected cases in which supine MRI/ radiographs are negative but symptoms indicate neurogenic claudication.12 It is crucial to recall that it is not a question of whether increased slip can be proven with either method, but rather if this information adds to the clinical decision-making regarding treatment. Prospective, appropriately powered studies are warranted to better assess the utility of functional MRI in the detection and evaluation of stenosis in the setting of DS.1
COMPUTED TOMOGRAPHY (CT) AND DS
With development of the MRI technique, providing more detailed anatomic information without radiation, the value of computed tomography (CT) with regard to DS has diminished. CT may however still be of value, primarily to assess details regarding bony structures such as degenerative changes of the facet joints and bony spurs protruding into the spinal canal causing central and forminal narrowing (Fig. 2-7).22 In patients with contraindications for MRI, in whom clinicians suspect DS with accompanying spinal and/or foraminal stenosis, CT myelography is recommended.1,2,14,22 CT myelography may also be valuable postoperatively, when artifacts from surgical hardware often restrict the MRI assessment.22 High radiation exposure, the former drawback of CT, has decreased since both hardware and software CT equipment are continuously developing. Therefore “low dose CT protocols,” which decrease the radiation dose without sacrificing image quality, might become potential tools to evaluate spinal biomechanics, since they provide the possibility to obtain spinal images in three-dimensions with high resolution.73-75 For example, Försth et al. have reported that three-dimensional (3D) CT provides a tool for measuring spinal 3D movements safely, reliably and with high accuracy.76
REFERENCES
- Matz PG, Meagher RJ, Lamer T, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 2016;16(3):439-448.
- Thornhill BA, Green DJ, Schoenfeld AH. Imaging techniques for the diagnosis of spondylolisthesis. In: Wollowick A, Sarwahi V, eds. Spondylolisthesis. Boston, MA: Springer; 2015:59-94.
- O’Dell MC, Kohler NJ, Harshman BK, et al. Degenerative disease of the spine and other spondyloarthropathies. In: Saba L, ed. Imaging of the Pelvis, Musculoskeletal System, and Special Applications to CAD. Boca Raton, FL: Taylor & Francis Group, LLC; 2016:179-203.
- Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335.
- Butt S, Saifuddin A. The imaging of lumbar spondylolisthesis. Clin Radiol. 2005;60(5):533-546.
- Postacchini F, Perugia D. Degenerative lumbar spondylolisthesis. Part I: etiology, pathogenesis, pathomorphology, and clinical features. Ital J Orthop Traumatol. 1991;17(2):165-173.
- Cinotti G, Postacchini F, Fassari F, Urso S. Predisposing factors in degenerative spondylolisthesis. A radiographic and CT study. Int Orthop. 1997;21(5):337-342.
- Kalichman L, Kim DH, Li L, Guermazi A, Berkin V, Hunter DJ. Spondylolysis and spondylolisthesis: prevalence and association with low back pain in the adult community-based population. Spine. 2009;34(2):199-205.
- Degenerative lumbar spondylolisthesis: an epidemiological perspective: the Copenhagen Osteoarthritis Study. Spine. 2007;32(1):120-125.
- Lehmann T, Brand R. Instability of the lower lumbar spine. Orthop Trans. 1983;7(97):155-163.
- Berlemann U, Jeszenszky DJ, Bühler DW, Harms J. Mechanisms of retrolisthesis in the lower lumbar spine. A radiographic study. Acta Orthop Belg. 1999;65(4):472-477.
- Jayakumar P, Nnadi C, Saifuddin A, Macsweeney E, Casey A. Dynamic degenerative lumbar spondylolisthesis: diagnosis with axial loaded magnetic resonance imaging. Spine. 2006;31(10):E298-301.
- Otani K, Okawa A, Shinomiya K, Nakai O. Spondylolisthesis with postural slip reduction shows different motion patterns with video-fluoroscopic analysis. J Orthop Sci. 2005;10(2):152-159.
- Watters WC 3rd, Bono CM, Gilbert TJ, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 2009;9(7):609-614.
- Hammouri QM, Haims AH, Simpson AK, Alqaqa A, Grauer JN. The utility of dynamic flexion-extension radiographs in the initial evaluation of the degenerative lumbar spine. Spine. 2007;32(21):2361-2364.
- Koreckij TD, Fischgrund JS. Degenerative spondylolisthesis. J Spinal Disord Tech. 2015;28(7):236-241.
- Friberg O. Functional radiography of the lumbar spine. Ann Med. 1989;21(5):341-346.
- Segebarth B, Kurd MF, Haug PH, Davis R. Routine upright imaging for evaluating degenerative lumbar stenosis: incidence of degenerative spondylolisthesis missed on supine MRI. J Spinal Disord Tech. 2015;28(10):394-397.
- Kanno H, Ozawa H, Koizumi Y, et al. Changes in lumbar spondylolisthesis on axial-loaded MRI: do they reproduce the positional changes in the degree of olisthesis observed on X-ray images in the standing position? Spine J. 2015;15(6):1255-1262.
- Nizard RS, Wybier M, Laredo JD. Radiologic assessment of lumbar intervertebral instability and degenerative spondylolisthesis. Radiol Clin North Am. 2001;39(1):55-71, v-vi.
- Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L. Lumbar intervertebral instability: a review. Radiology. 2007;245(1):62-77.
- Siemund R, Thurnher M, Sundgren PC. How to image patients with spine pain. Eur J Radiol. 2015;84(5):757-764.
- Kepler CK, Hilibrand AS, Sayadipour A, et al. Clinical and radiographic degenerative spondylolisthesis (CARDS) classification. Spine J. 2015;15(8):1804-1811.
- Beck NA, Miller R, Baldwin K, et al. Do oblique views add value in the diagnosis of spondylolysis in adolescents? J Bone Joint Surg Am. 2013;95(10):e65.
- Dupuis PR, Yong-Hing K, Cassidy JD, Kirkaldy-Willis WH. Radiologic diagnosis of degenerative lumbar spinal instability. Spine. 1985;10(3):262-276.
- Meyerding, HW. Spondylolisthesis. Surg Gynecol Obstet. 1932;54:371-377.
- Taillard W. [Spondylolisthesis in children and adolescents]. Acta Orthop Scand. 1954;24(2):115-144.
- Danielson B, Frennered K, Irstam L. Roentgenologic assessment of spondylolisthesis. I. A study of measurement variations. Acta Radiol. 1988;29(3):345-351.
- Danielson B, Frennered K, Selvik G, Irstam L. Roentgenologic assessment of spondylolisthesis. II. An evaluation of progression. Acta Radiol. 1989;30(1):65-68.
- Norton RP, Bianco K, Klifto C, Errico TJ, Bendo JA. Degenerative spondylolisthesis: an analysis of the nationwide inpatient sample database. Spine. 2015;40(15):1219-1227.
- Försth P, Ólafsson G, Carlsson T, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med. 2016;374(15):1413-1423.
- Matsunaga S, Sakou T, Morizono Y, Masuda A, Demirtas AM. Natural history of degenerative spondylolisthesis. Pathogenesis and natural course of the slippage. Spine. 1990;15(11):1204-1210.
- Maigne JY, Lapeyre E, Morvan G, Chatellier G. Pain immediately upon sitting down and relieved by standing up is often associated with radiologic lumbar instability or marked anterior loss of disc space. Spine. 2003;28(12):1327-1334.
- Boden SD, Wiesel SW. Lumbosacral segmental motion in normal individuals. Have we been measuring instability properly? Spine. 1990;15(6):571-576.
- Câmara JR, Keen JR, Asgarzadie F. Functional radiography in examination of spondylolisthesis. AJR Am J Roentgenol. 2015;204(4):W461-W469.
- Pitkänen MT, Manninen HI, Lindgren KA, Sihvonen TA, Airaksinen O, Soimakallio S. Segmental lumbar spine instability at flexion-extension radiography can be predicted by conventional radiography. Clin Radiol. 2002;57(7):632-639.
- Penning L, Blickman JR. Instability in lumbar spondylolisthesis: a radiologic study of several concepts. AJR Am J Roentgenol. 1980;134(2):293-301.
- Shaffer WO, Spratt KF, Weinstein J, Lehmann TR, Goel V. 1990 Volvo Award in clinical sciences. The consistency and accuracy of roentgenograms for measuring sagittal translation in the lumbar vertebral motion segment. An experimental model. Spine. 1990;15(8):741-750.
- Simmonds AM, Rampersaud YR, Dvorak MF, Dea N, Melnyk AD, Fisher CG. Defining the inherent stability of degenerative spondylolisthesis: a systematic review. J Neurosurg Spine. 2015;23(2):178-189.
- Hayes MA, Howard TC, Gruel CR, Kopta JA. Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine. 1989;14(3):327-331.
- Tallroth K, Alaranta H, Soukka A. Lumbar mobility in asymptomatic individuals. J Spinal Disord. 1992;5(4):481-484.
- Cho BY, Murovic JA, Park J. Imaging correlation of the degree of degenerative L4-5 spondylolisthesis with the corresponding amount of facet fluid. J Neurosurg Spine. 2009;11(5):614-619.
- Kanemura A, Doita M, Kasahara K, Sumi M, Kurosaka M, Iguchi T. The influence of sagittal instability factors on clinical lumbar spinal symptoms. J Spinal Disord Tech. 2009;22(7):479-485.
- Splendiani A, Perri M, Grattacaso G, et al. Magnetic resonance imaging (MRI) of the lumbar spine with dedicated G-scan machine in the upright position: a retrospective study and our experience in 10 years with 4305 patients. Radiol Med. 2016;121(1):38-44.
- Iguchi T, Wakami T, Kurihara A, Kasahara K, Yoshiya S, Nishida K. Lumbar multilevel degenerative spondylolisthesis: radiological evaluation and factors related to anterolisthesis and retrolisthesis. J Spinal Disord Tech. 2002;15(2):93-99.
- Cabraja M, Mohamed E, Koeppen D, Kroppenstedt S. The analysis of segmental mobility with different lumbar radiographs in symptomatic patients with a spondylolisthesis. Eur Spine J. 2012;21(2):256-261.
- Wood KB, Popp CA, Transfeldt EE, Geissele AE. Radiographic evaluation of instability in spondylolisthesis. Spine. 1994;19(15):1697-1703.
- Landi A, Gregori F, Marotta N, Donnarumma P, Delfini R. Hidden spondylolisthesis: unrecognized cause of low back pain? Prospective study about the use of dynamic projections in standing and recumbent position for the individuation of lumbar instability. Neuroradiology. 2015;57(6):583-588.
- Pitkänen M, Manninen H. Sidebending versus flexion-extension radiographs in lumbar spinal instability. Clin Radiol. 1994;49(2):109-114.
- Pitkänen M, Manninen HI, Lindgrer KA, Turunen M, Airaksinen O. Limited usefulness of traction-compression films in the radiographic diagnosis of lumbar spinal instability. Comparison with flexion-extension films. Spine. 1997;22(2):193-197.
- Blumenthal C, Curran J, Benzel EC, et al. Radiographic predictors of delayed instability following decompression without fusion for degenerative grade I lumbar spondylolisthesis. J Neurosurg Spine. 2013;18(4):340-346.
- Knutsson F. The instability associated with disk degeneration in the lumbar spine. Acta Radiol. 1944;25(5-6):593-609.
- Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995;8(6):464-473.
- Friberg O. Lumbar instability: a dynamic approach by traction-compression radiography. Spine. 1987;12(2):119-129.
- Putto E, Tallroth K. Extension-flexion radiographs for motion studies of the lumbar spine. A comparison of two methods. Spine. 1990;15(2):107-110.
- Kälebo P, Kadziolka R, Swärd L, Zachrisson BE. Stress views in the comparative assessment of spondylolytic spondylolisthesis. Skeletal Radiol. 1989;17(8):570-575.
- Dvorák J, Panjabi MM, Novotny JE, Chang DG, Grob D. Clinical validation of functional flexion-extension roentgenograms of the lumbar spine. Spine. 1991;16(8):943-950.
- Carrino JA, Lurie JD, Tosteson AN, et al. Lumbar spine: reliability of MR imaging findings. Radiology. 2009;250(1):161-170.
- Sengupta DK, Herkowitz HN. Degenerative spondylolisthesis: review of current trends and controversies. Spine. 2005;30(6 Suppl):S71-81.
- McGregor AH, Anderton L, Gedroyc WM, Johnson J, Hughes SP. The use of interventional open MRI to assess the kinematics of the lumbar spine in patients with spondylolisthesis. Spine. 2002;27(14):1582-1586.
- Steurer J, Roner S, Gnannt R, Hodler J; LumbSten Research Collaboration. Quantitative radiologic criteria for the diagnosis of lumbar spinal stenosis: a systematic literature review. BMC Musculoskelet Disord. 2011;12:175.
- Chaput C, Padon D, Rush J, Lenehan E, Rahm M. The significance of increased fluid signal on magnetic resonance imaging in lumbar facets in relationship to degenerative spondylolisthesis. Spine. 2007;32(17):1883-1887.
- Lattig F, Fekete TF, Grob D, Kleinstück FS, Jeszenszky D, Mannion AF. Lumbar facet joint effusion in MRI: a sign of instability in degenerative spondylolisthesis? Eur Spine J. 2012;21(2):276-281.
- Mamisch N, Brumann M, Hodler J, et al. Radiologic criteria for the diagnosis of spinal stenosis: results of a Delphi survey. Radiology. 2012;264(1):174-179.
- Barz T, Melloh M, Staub LP, et al. Nerve root sedimentation sign: evaluation of a new radiological sign in lumbar spinal stenosis. Spine. 2010;35(8):892-897.
- Zhang L, Chen R, Xie P, Zhang W, Yang Y, Rong L. Diagnostic value of the nerve root sedimentation sign, a radiological sign using magnetic resonance imaging, for detecting lumbar spinal stenosis: a meta-analysis. Skeletal Radiol. 2015;44(4):519-527.
- Caterini R, Mancini F, Bisicchia S, Maglione P, Farsetti P. The correlation between exaggerated fluid in lumbar facet joints and degenerative spondylolisthesis: prospective study of 52 patients. J Orthop Traumatol. 2011;12(2):87-91.
- Oishi Y, Murase M, Hayashi Y, Ogawa T, Hamawaki J. Smaller facet effusion in association with restabilization at the time of operation in Japanese patients with lumbar degenerative spondylolisthesis. J Neurosurg Spine. 2010;12(1):88-95.
- Snoddy MC, Sielatycki JA, Sivaganesan A, Engstrom SM, McGirt MJ, Devin CJ. Can facet joint fluid on MRI and dynamic instability be a predictor of improvement in back pain following lumbar fusion for degenerative spondylolisthesis? Eur Spine J. 2016;25(8):2408-2415.
- Ferreiro Perez A, Garcia Isidro M, Ayerbe E, Castedo J, Jinkins JR. Evaluation of intervertebral disc herniation and hypermobile intersegmental instability in symptomatic adult patients undergoing recumbent and upright MRI of the cervical or lumbosacral spines. Eur J Radiol. 2007;62(3):444-448.
- Ozawa H, Kanno H, Koizumi Y, et al. Dynamic changes in the dural sac cross-sectional area on axial loaded MR imaging: is there a difference between degenerative spondylolisthesis and spinal stenosis? AJNR Am J Neuroradiol. 2012;33(6):1191-1197.
- Hansson T, Suzuki N, Hebelka H, Gaulitz A. The narrowing of the lumbar spinal canal during loaded MRI: the effects of the disc and ligamentum flavum. Eur Spine J. 2009;18(5):679-686.
- Svedmark P, Weidenhielm L, Nemeth G, et al. Model studies on segmental movement in lumbar spine using a semi-automated program for volume fusion. Comput Aided Surg. 2008;13(1):14-22.
- Svedmark P, Tullberg T, Noz ME, et al. Three-dimensional movements of the lumbar spine facet joints and segmental movements: in vivo examinations of normal subjects with a new non-invasive method. Eur Spine J. 2012;21(4):599-605.
- Svedmark P, Berg S, Noz ME, et al. A new CT method for assessing 3D movements in lumbar facet joints and vertebrae in patients before and after TDR. Biomed Res Int. 2015;2015:260703.
- Försth P. On surgery for lumbar spinal stenosis. In: Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1135. Uppsala, Sweden: Acta Universitatis Upsaliensis; 2015.