Timo Stubig, Michael Grevitt, Christian W. Mueller
INTRODUCTION
Thoracic and thoracolumbar injuries with significant vertebral comminution and/or ligamentous instability may result in mechanical instability or compression of neural elements. The optimal therapy for thoracolumbar and lumbar spine fractures is not clear. Although different countries and institutions claim to provide optimal care, the evidence is largely based on retrospective case series.1-3 Even for the common burst fracture, there is lack of consensus on whether to treat by surgery or by non-operative means.1-11 Several operative methods exist to achieve fracture reduction and fixation, but none of them has had a proven advantage in terms of patient outcome in comparison with the others.3
HISTORY OF ANTERIOR APPROACHES AND CURRENT CONCEPTS
Historically, the initial treatment of lumbar fractures involved prolonged bedrest, which has proven to be associated with a high mortality rate.12 Posterior stabilization techniques were developed to expedite rehabilitation.13-18 Problems of hardware failure and recurrence of deformity12,13,19,20 and persistent bony fragments in the spinal canal after posterior stabilization led to the development of anterior stabilization and decompression techniques.21-25 Paul et al.,26 Dunn and Kaneda,26-28 and McAffee and Bohlman21,29 were the earliest authors to publish studies of spinal stabilization for thoracolumbar fractures using an anterior approach.12 Combined anterior and posterior techniques were subsequently described with the aim to stabilize fractures in different planes and to prevent further adjacent segment degeneration and late kyphosis.30-42
McCormack et al.43 described the widely quoted “load-sharing” classification in 1994. Through that classification system, we can use CT images to assist in decision making, e.g., whether to do a posterior short segment fixation for less complex injuries or combined posterior and anterior fixation for more comminuted injuries.44
With the current upward trend of minimally invasive surgery (MIS) in all aspects of surgery, less invasive anterior techniques using thoracoscopy, laparoscopy or microscopy have evolved.45-55 The extreme lateral interbody fusion (XLIF) corprectomy (X-CORE) technique is a minimally invasive modification of the classic retroperitoneal approach to the lumbar spine and the XLIF procedure, which was first presented in 2001 by Pimenta56 and adopted by Ozgur et al. in 2006.57
Some authors have described a posterior approach based on degenerative spine surgery techniques. The combined anterior stabilization using the PLIF (Posterior lumbar interbody fusion) was first attempted by Cloward et al. in 195458 and later revised by Lin et al.59 Another technique, the TLIF (transforaminal interbody lumbar fusion) procedure,60-62 was first described by Harms et al. in 1992.63
INDICATIONS AND THERAPEUTIC OPTIONS
Therapeutic options for lumbar burst fractures or associated ligamentous injuries depend on radiological and clinical findings as well as comorbidities. These include:
- Conservative treatment including bed rest, bracing or early mobilization;
- Isolated dorsal stabilization (with or without decompression and with or without fusion, open or minimally invasive);
- Isolated anterior stabilization; and
- Combined anterior (cages, bone grafts, ns or rods) and posterior procedures (single or two-staged procedure).
General goals for surgery should include appropriate decompression of neural elements, facilitation of neurological recovery, restoration of the spinal alignment if comminuted and prevention of secondary loss of correction and restoration of spinal stability.64 Moreover instrumentation should be as short as biomechanically feasible and should allow rapid mobilization and rehabilitation to decrease problems of prolonged immobilization.65 While an anterior approach allows for direct visualization of the spinal canal during decompression and restoration of ventral load-bearing capacity through placement of a strut graft, plates or cages, dorsal fixation involves constructs that restore the dorsal tension band and three-point bending forces to the spine to resist progressive kyphosis and load sharing between anterior and posterior columns.64
There are several studies showing positive outcomes for every kind of treatment1,20,66-73 whereas better radiologic and biomechanically stable results are achieved with anterior and posterior fusion.35,70 Short segment instrumentation with pedicle screws placed only in the vertebrae above and below the fracture has been associated with a higher rate of construct failure ranging from 9 to 54%13,20,66,74-77 as well as an post-operative kyphosis ranging from 3° to 12°.12 For thoracolumbar fractures, the AO classification is widely used.56 While A1 and A2 fractures can be treated conservatively or with by posterior stabilization only, the optimal strategy for A3 and A4 is unclear.1,3,20,72,75,78-83
Overall anterior and posterior surgery is most often used in unstable burst fractures with severe bony destruction or discoligamentous injury.1,12,35,67,70,71,84,85 Whitesides86 wrote that single dorsal fusion in unstable vertebral body fractures with or without ligamentous instability may fail and recommended the support of the anterior column via an anterior approach using the ribs, fibula or tricortical iliac strut graft.87
Instability may be present if there was greater than 15 to 25° of local kyphosis,88,89 an interspinous widening of more than 7 mm,23,73,92 translational subluxation of more than 3 mm, significant comminution of the fractured vertebral body with reduced anterior vertebral body height of more than 50%12, 91 normal alignment of the facet joints.90
While AO type A3 fractures may be treated by posterior stabilization and anterior monosegmental fixation, A4 fractures (burst fractures) and A2 pincer fractures may be treated by bisegmental corpectomy and stabilization.92
For B1 fractures with pure bony rupture and B3 injuries, posterior stabilization may be sufficient, whereas as B2 and C fractures of the lumbar spine may be treated by combined anterior and posterior stabilization.92-94
However, anterior surgery alone may fail in cases with disrupted posterior stabilizing elements in B2 and C Type injuries.73 If a stand-alone anterior construct is planned, any disruption of posterior ligamentous structures should be excluded with the use of MRI (magnet resonance imaging).73,92
Furthermore a stable anterior construct with cage and the use of an fixed-angle stable plate may be used, and the surgeon has to keep in mind that sometimes, when doing surgery in a AO Type A injury, intraoperative an AO type B injury is found due to lengthening or disruption of the posterior tension band,91 which was not visible in preoperative MRI or CT.
In summary indications for anterior stabilizations include compromised load-bearing capacity of the ventral spine by fracture or, after decompression, disruption of dorsal ligaments and the tension band as shown by facet dislocation or fracture with instability in several planes. Other indications include delayed treatment of injuries, including late posttraumatic deformities, and anterior neural compression or incomplete spinal cord injury.87,95-98
Nevertheless, decision making should include patient’s biological age, clinical symptoms, occurrence of neurologic symptoms, co-morbidities such as cancer and osteoporosis, and infections and is further dependent on personal competencies, institutional facilities and/or regional circumstances.
TIMING OF SURGERY
Posterior stabilization represents the utilitarian approach for emergency procedures and may be applied to highly unstable AO type B and C injuries, as well as A3 and A4 injuries with neurologic impairment, given the necessity of immediate surgery.92 Ventral stabilization is usually done at a second stage after taking care of other injuries.
SURGICAL TECHNIQUES
Surgical techniques for anterior spine stabilization can be divided into one stage combined posterior stabilization with anterior cage implantation (PLIF or TLIF and lateral extracavitary approach (LECA)) and anterior procedures with anterior discectomy, decompression, corpectomy and stabilization.
One Staged Combined Anterior/Posterior Procedures
PLIF/TLIF
For both procedures, the patient is placed in prone position on a radiolucent operation table.63 A standard posterior midline approach is used to access the vertebrae with preservation of the supraspinous and interspinous ligaments and subperiosteal exposure of the spine. Pedicle screws are inserted in the appropriate vertebrae. For the TLIF procedure, the pars interarticularis is removed, and a hemifacetectomy performed. For the PLIF procedure for the levels L3–S1, the approach should be extended to the superior articular process and resection of the lower part of the inferior articular process of the upper vertebra performed. At the thoracolumbar junction the articular processes have to be completely resected in order to access the disc space via the foramina.87 In both cases the dural sac is identified and carefully retracted no further than the midline in the lumbar region. The disc space and the retro-pulsed bony fragment are identified.87 After identification of the lower and upper nerve root, a discectomy is performed. Occasionally, endplate osteophytes need to be removed. After decortication of the endplate, the next step is a distraction of the disc space. In the prepared space, either previously acquired cortical bone grafts from the posterior iliac crests61,87 or cages filled with autologous cancellous bone from the iliac crest may be inserted.99 After that, the distraction is relaxed, and rods, contoured to the appropriate size and angle, are attached to the pedicle screws.99 The intervertebral space is then slightly compressed, and the screws are tightened. Finally, an interspinous and interlaminar spondylodesis is usually performed in the open technique.67,87,100
Although there are various reports about minimal invasive percutaneous pedicle screw placement for trauma cases101-103 and MIS TLIF for degeneration,104-106 there is no evidence based data available describing minimal invasive TLIF procedures in trauma.
LECA
The lateral extracavitary approach (LECA) was introduced by Capener107 and modified by Larson et al.108 Following a semicircular skin incision of with a radius of 10-12 cm, including the resection of the transversus process, the costotransverse joint, the pedicle and at least one rib,109 it offers the advantage of single stage, single incision, ventral and dorsal exposure and stabilization of the spine64 and also the theoretical benefit of reduced patient morbidity because of the avoidance of a second procedure. Nevertheless, its application in spine trauma is limited to special cases.
Anterior Procedures
Anterior spine surgery usually follows the same steps, only differing in the approaches to the anterior approaches depending on the anatomic level. The approaches can be divided in approaches to the thoracolumbar junction (Th10-L1) and those of the lumbar region (L3-S1). Anterior approaches to L2 are different; the right approach is based on specific anatomical conditions and borrows techniques from the levels above and below.110
Almost all surgical procedures follow the same surgical steps:
- Surgical Approach,
- Discectomy,
- Partial corpectomy/ corpectomy, and
- Stabilization.
Discectomy
Discectomy is always performed before removal of the vertebral body, because it allows visualization the upper and lower limit of the spinal canal. In the case of a partial corpectomy, i.e. for monosegmental fusion, discectomy is performed for the disc adjacent to the fractured end plate. For a complete corpectomy with bisegmental fusion, the disc of both adjacent intervertebral spaces has to be removed.111
Partial or total corpectomy
Prior to corpectomy, the segmental vessels have to be identified. In some cases, these might already be disrupted due to trauma; however, these should be ligated in the midline of the vertebral body. Following that, a corpectomy or partial corpectomy is performed. Starting with the fractured portion with a combination of rongeurs and osteotomes, a rim of the vertebral body is left anteriorly to facilitate fusion. The anterior longitudinal ligament is regularly spared in acute fracture cases. In older fractures (over 4 weeks) or in malunions, a complete release of the anterior longitudinal ligament and circumferential annular release may be necessary to regain anterior alignment.12 The posterior portion of the vertebral body is removed with a burr. After this the posterior wall is resected, and the spinal canal decompressed by removing retropulsed bone fragments. The excavated bone fragments should be reserved for later bone fusion.111
Stabilization
Anterior column reconstruction and stabilization of the vertebral body following a partial corpectomy can be performed using an autograft or allograft (Fig. 5-1), strut graft combined with a plate (Fig. 5-2) or a synthetic or metallic cage (Fig. 5-3, expandable or non-expandable or Fig. 5-4). For complete corpectomies, usually expandable cages filled with cancellous bone and material from the comminuted vertebral fracture or the removed rib or an expendable cage with anatomic endplate and lateral addition of the previously prepared cancellous bone is used.111 While the autograft solution, sometimes combined with a cage may be used for A3 fractures with partial corprectomy in younger patients, older patients or those that require more extensive corprectomy may be treated more often with the use of an expendable cage (Fig. 5-3 and 5-4).73



The patient was treated by two staged posterior first and later anterior lumbar spine surgery with mini open lumbotomy, corpectomy and cage implantation as well as addition of cancellous bone laterally.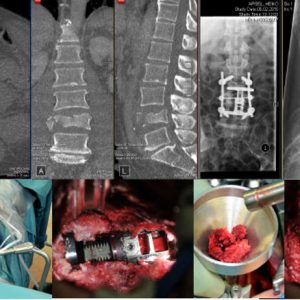
Two staged procedure with percutaneous posterior stabilization and minimal invasive X-CORE procedure after 6 weeks. The procedure was uneventful.
Approaches
As previously described, there are different approaches depending on the anatomic height of the affected vertebral bodies. For the thoracolumbar junction (Th10-L1/2), usually a right or left sided thoracotomy can be used in the classic open or mini-open approach as well as thoracoscopic approaches. In special occasions, a thoraco phrenolumbotomy is performed.
For lumbar anterior stabilization between levels L2 and L5, usually an open lumbotomy suffices for most injuries, while a mini lumbotomy or XLIF approach is used in special cases. At the lumbosacral junction a retroperitoneal approach in supine position with a classic abdominal midline incision or mini-open procedure may be used,111 although there is no description for the use of this technique in trauma in the literature.
Surgical technique thoracolumbar junction
Thoracotomy and thoracoscopic procedures are can be performed to L2, whereas below L2 level a mini-lumbotomy may be necessary, which is described in the previous section. Nevertheless, in the recent years, mini-open or endoscopic procedures have gained popularity.92,112 The procedure can be performed in prone or lateral position with lateral position being the standard position.112 The left hip is flexed to decrease psoas tension, and a pillow is placed between the legs.12
The side of the approach (right or left side) can be decided based upon the location of the major vessels, which can be identified by the preoperative CT scan, with left side being preferred for the thoracolumbar region.12
Anaesthetic preparations include venous and artery catheters and a double lumen tube. After positioning on the table, fluoroscopic x-rays are obtained to assure free c-arm flouroscopy movement. Under radiologic control, the injured segments are marked on the skin. For the thoracoscopic procedure (see Fig. 5-1), usually 3 or 4 small incisions (1x 3.5 cms long, the rest usually 1-2 cms are used, the location is usually dependent on the surgeon’s preferences. The first incision is performed by preparation whereas the other 3 incisions are performed under thoracoscopic control.
For thoracotomy the incision is carried out from postero-superiorly around the angle of the scapula, obliquely sloping to antero-inferiorly.111 The length of the incision depends on many factors (e.g., number, location and classification of fractures; obesity of the patient; previous thoracic operations) and should be planned to be two levels above the fractured level.111 After incision of the subcutaneous fat, sometimes the dissection and removal of a rib is necessary, which should be used for later bone grafting.111 After that, the pleura is cut, and the lung is retracted. For L1 and L2 levels, a diaphragm split is usually performed.112 Then, subperiosteal exposure of the lateral aspect of the vertebral body is performed from the midline anteriorly to the lateral aspect of the pedicle posteriorly.12 After decompression, corpectomy and stabilization of the vertebral body, a thorax drain is inserted.
For the thoraco phrenolumbotomy, the incision is usually centered over the fractured vertebra after identification with the c-arm. The length of the incision depends on many factors, and it is made over a rib, usually the rib attached to the vertebra two levels above the fractured vertebra.111 After the skin incision, chest and abdominal muscles distal to the costal cartilage are incised with cautery. The latissimus dorsi can usually be spared by retracting it posteriorly. The rib is exposed subperiosteally and usually resected and saved for subsequent bone grafting. The pleura parietalis is opened posteriorly, and the lung exposed. At the anterior part of the incision, the three muscle layers of the abdominal wall are split and the retroperitoneal cavity is exposed. For access to the T12/L1 junction, the diaphragm has to be cut close to the chest wall.111 The diaphragm is then retracted anteriorly to join the retroperitoneal space and the intrapleural cavity. There is no need for lung collapse on the side of surgery. To expose vertebrae below L1, the peritoneum is retracted anteriorly, and the lumbotomy is performed.111
Surgical technique lumbar region
For the lumbotomy, in lateral position, as well as for other approaches, the incision depends on the fracture level, which should be correlated with preoperative and c-arm imaging. Overall, three vertebrae can be easily accessed. The subcutaneous tissue and the fascia as well as the three abdominal wall muscles, the external abdominal oblique muscle, the internal abdominal oblique muscle and the transverse abdominal muscle are incised. The incision should subperiosteally expose the distal 5 cm of the 12th rib, which is excised afterwards. After incision of the transversalis fascia, the retroperitoneal fat is visible as a landmark to the retroperitoneal space. The peritoneum has to be mobilized until the psoas muscle is exposed, which is then retracted and mobilized. After dissection of the segmental vessels and the intervertebral disc space, the vertebral body above and below the fractured vertebra should be exposed.111 Care must be taken of the common iliac vessels, especially at the level of L4 and below.
For the mini-lumbotomy (see illustrative case in Fig. 5-3), the fractured vertebra and the adjacent vertebrae are marked on the skin with c-arm fluoroscopy in lateral position. Specific instruments, i.e., a self-retaining retractor system and implants, are needed. For bisegmental stabilization, the incision runs from the posterior edge of the lower end plate of the vertebral body above the fracture to the anterior edge of the upper endplate of the fractured vertebra. For a monosegmental stabilization, the incision runs from the midpoint of the posterior wall of the vertebral body above the fracture to the midpoint of the anterior wall of the vertebral body below the fracture.
The incision is performed in the same way as the classic lumbotomy. After release of the psoas muscle and retraction, a self-retaining retractor system is positioned, and, after the ligature of the vessels and discectomy, the corpectomy is performed. For transmuscular incision of the psoas and retraction, neuromonitoring is recommended.
For the extreme lateral interbody fusion (XLIF or X-Core, see Fig. 5-4), the patient is placed in right lateral position with the left side elevated and flexed to increase the distance between the iliac crest and the rib cage. With c-arm flouroscopy, a k-wire and lateral fluoroscopic image are used to identify the vertebra’s mid-point. One skin mark is made on the patient’s lateral side, over the affected vertebra, and a second mark posterior to this first mark at the border between the erector spinae muscles and the abdominal obliques. At this second mark, a longitudinal incision of about 2 cm is made to accommodate the surgeon’s index finger which is inserted anteriorly through the muscle layers to identify the retroperitoneal space.
After accessing the retroperitoneal fat, the index finger is turned towards the skin, and a skin incision is made. An initial dilatator is introduced, the psoas muscle is dissected with neuromonitoring control57 between the middle and anterior third of the muscle, ensuring that the nerves of the lumbar plexus are located posteriorly and outside the operative corridor. C-Arm images should confirm the definitive position. Other dilatators with increasing diameters are introduced; after the final dilatator, a retractor system is positioned. After vessel ligature, the vertebral body can be exposed.57
Complications in Anterior Lumbar Spine Surgery
Overall, the combined rate of complications after posterior and anterior was reported to be up to 50%,113 while other authors in recent years report a cumulative complication rate of 10-16%.1,22 PLIF and TLIF procedures are to be associated with a high overall of complication, up to 25% for the PLIF procedure.99 Furthermore significant rate of neurologic injury secondary to the retraction and manipulation of the neural elements that are required to access the disc space in up to 10% of the cases as well as implant failure is described for the PLIF procedure.65,114,115
In anterior spine surgery, general complications include infection, thrombosis, lung artery embolus, non-fusions, loss of reduction with or without implant dislocation, cosmetic changes, persistent pain or neurology as well as pneumonia, postoperative ileus.116 One of the most dramatic complications overall is bleeding of big vessels, i.e., aortic bleeding; while bleeding of the iliac vessels also needs immediate treatment,117, 118 these have a single complication rate of up to 15% of the cases of anterior lumbar surgery.
Although approach morbidity decreased with the evolution of minimally invasive surgery, there are still some typical complications for anterior spine surgery. Typical complications for thoracotomy, thoracoscopic procedures or lumbotomy with incision of the diaphragm include pleura effusion, haemothorax or pneumothorax, dura leakage and respiratory insufficiency as well as empyema. Furthermore, damage to the kidneys, spleen, liver or intestine117 can occur.116
For retroperitoneal approaches like lumbotomy and XLIF/X-Core, specific complications such as postoperative pain and weakness in the M. psoas with transient numbness along the genitofemoral nerve are described as well as other injuries to the lumbar plexus57, 119, 120 including retrograde ejaculation.121 More complications for these procedures are abdominal wall hernia, lymphocele and ureter injury.116, 122
- Knop C, Blauth M, Bühren V, et al. [Surgical treatment of injuries of the thoracolumbar transition--3: Follow-up examination. Results of a prospective multi-center study by the “Spinal” Study Group of the German Society of Trauma Surgery]. Unfallchirurg, 2001;104(7):583-600.
- Trivedi JM. Spinal trauma: therapy—options and outcomes. Eur J Radiol. 2002;42(2):127-134.
- Verlaan JJ, Diekerhof CH, Buskens E, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine (Phila Pa 1976). 2004;29(7):803-814.
- Aras EL, Bunger C, Hansen ES, Sogaard R. Cost-Effectiveness of surgical versus conservative treatment for thoracolumbar burst fractures. Spine (Phila Pa 1976). 2016;41(4):337-343.
- Archavlis E, Papadopoulos N, Ulrich P. Corpectomy in destructive thoracolumbar spine disease: cost-effectiveness of 3 different techniques and implications for cost reduction of delivered care. Spine (Phila Pa 1976). 2015;40(7):E433-438.
- Dai LY, Jiang LS, Jiang SD. Conservative treatment of thoracolumbar burst fractures: a long-term follow-up results with special reference to the load sharing classification. Spine (Phila Pa 1976). 2008;33(23):2536-2544.
- de Klerk LW, Fontijne WP, Stijnen T, Braakman R, Tanghe HL, van Linge B. Spontaneous remodeling of the spinal canal after conservative management of thoracolumbar burst fractures. Spine (Phila Pa 1976). 1998;23(9):1057-60.
- Jaffray DC, Eisenstein SM, Balain B, Trivedi JM, Newton Ede M. Early mobilisation of thoracolumbar burst fractures without neurology: a natural history observation. Bone Joint J. 2016;98-B(1):97-101.
- Schroeder GD, Vaccaro AR, Kepler CK, et al. Establishing the injury severity of thoracolumbar trauma: confirmation of the hierarchical structure of the AOSpine Thoracolumbar Spine Injury Classification System. Spine (Phila Pa 1976). 2015;40(8):E498-503.
- Vorlat P, Leirs G, Tajdar F, Hulsmans H, De Boeck H, Vaes P. Predictors of recovery after conservative treatment of AO-type A thoracolumbar spine fractures without neurological deficit. Spine (Phila Pa 1976). 2010;43(2):141-147.
- Willen J, Lindahl S, Nordwall A. Unstable thoracolumbar fractures. A comparative clinical study of conservative treatment and Harrington instrumentation. Spine (Phila Pa 1976). 1985;10(2):111-122.
- McDonough PW, Davis R, Tribus C, Zdeblick TA. The management of acute thoracolumbar burst fractures with anterior corpectomy and Z-plate fixation. Spine (Phila Pa 1976). 2004;29(17):1901-1908.
- Benson DR, Burkus JK, Montesano PX, Sutherland TB, McLain RF. Unstable thoracolumbar and lumbar burst fractures treated with the AO fixateur interne. J Spinal Disorders. 1992;5(3):335-343.
- Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976). 1992;17:317-324.
- Cresswell TR, Marshall PD, Smith RB. Mechanical stability of the AO internal spinal fixation system compared with that of the Hartshill rectangle and sublaminar wiring in the management of unstable burst fractures of the thoracic and lumbar spine. Spine (Phila 1976). 1998;23(1):111-115.
- Dick W. The “fixateur interne” as a versatile implant for spine surgery. Spine (Phila Pa 1976). 1987;12(9):882-900.
- Dick W, Kluger P, Magerl F, Woersdorfer O, Zach G. A new device for internal fixation of thoracolumbar and lumbar spine fractures: the 'fixateur interne'. Paraplegia. 1985;23(4):225-232.
- Sim E, Stergar PM. The fixateur interne for stabilising fractures of the thoracolumbar and lumbar spine. Int Orthop, 1992;16(4):322-329.
- Ebelke DK, Asher MA, Neff JR, Kraker DP. Survivorship analysis of VSP spine instrumentation in the treatment of thoracolumbar and lumbar burst fractures. Spine (Phila Pa). 1991;16(8):S428-432.
- Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976). 1992;17(5):528-540.
- Bohlman H, Freehafer A, Dejak J. Late anterior decompression of spinal-cord injuries. J Bone Joint Surg Am. 1975.
- Dimar JR 2nd , Wilde PH, Glassman SD, Puno RM, Johnson JR. Thoracolumbar burst fractures treated with combined anterior and posterior surgery. Am J Orthop (Belle Mead, NJ). 1996;25(2):159-165.
- Shono Y, McAfee PC, Cunningham BW. Experimental study of thoracolumbar burst fractures. A radiographic and biomechanical analysis of anterior and posterior instrumentation systems. Spine (Phila Pa).1994;19(15):1711-1722.
- Stolze D, Harms J. Kombinierte Stabilisationsverfahren an der thorako-lumbalen Wirbelsäule. Osteosynthese International. 1998;157-172.
- Ulmar B, Richter M, Kelsch G, Cakir B, Puhl W, Huch K. Distractible vertebral body replacement for the thoracic and lumbar spine. Acta Orthop Belg. 2005;71(4):467-471.
- Paul RL, Michael RH, Dunn JE, Williams JP. Anterior transthoracic surgical decompression of acute spinal cord injuries. Journal Neurosurg. 1975;43(3):299-307.
- Dunn HK. Anterior stabilization of thoracolumbar injuries. Clin Ortho Relat Res. 1984;189:116-124.
- Kaneda K, Abumi K, Fujiya M. Burst fractures with neurologic deficits of the thoracolumbar-lumbar spine. Results of anterior decompression and stabilization with anterior instrumentation. Spine (Phila Pa 1976). 1984;9(8):788-795.
- McAfee PC, Bohlman HH, Yuan HA. Anterior decompression of traumatic thoracolumbar fractures with incomplete neurological deficit using a retroperitoneal approach. J Bone Joint Surg Am. 1985;67(1):89-104.
- Been HD, Bouma GL. Comparison of two types of surgery for thoraco-lumbar burst fractures: combined anterior and posterior stabilisation vs. posterior instrumentation only. Acta Neurochir (Wien). 1999;141(4):349-357.
- Carl AL, Matsumoto M, Whalen JT. Anterior dural laceration caused by thoracolumbar and lumbar burst fractures. J Spinal Disord. 2000;13(5):399-403.
- Chung KJ, Eom SW, Noh KC, et al. Bilateral traumatic anterior dislocation of the hip with an unstable lumbar burst fracture. Clin Orthop Surg. 2009;1(2):114-117.
- Huang TJ, Chen JY, Shih HN, Chen YJ, Hsu RW. Surgical indications in low lumbar burst fractures: experiences with Anterior Locking Plate System and the reduction-fixation system. J Trauma, 1995;39(5):910-914.
- Kang CN, Cho JL, Suh SP, Choi YH, Kang JS, Kim YS. Anterior operation for unstable thoracolumbar and lumbar burst fractures: tricortical autogenous iliac bone versus titanium mesh cage. J Spinal Disord Tech. 2013;26(7):E265-271.
- Korovessis P, Baikousis A, Zacharatos S, Petsinis G, Koureas G, Iliopoulos P. Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (L2-L4) burst fractures. Spine (Phila Pa 1976). 2006;31(8):859-868.
- Kostuik JP. Anterior fixation for burst fractures of the thoracic and lumbar spine with or without neurological involvement. Spine (Phila Pa 1976). 1988;13(3):286-293.
- Ma JJ, Fan SW, Zhang J, Chen J, Zhao FD, Fang XQ. Anterior decompression and reconstruction for lumbar burst fractures. Orthop Surg. 2015;7(2):187-188.
- Miyakoshi N, Abe E, Shimada Y, Hongo M, Chiba M, Sato K. Anterior decompression with single segmental spinal interbody fusion for lumbar burst fracture. Spine (Phila Pa 1976). 1999;24(1):67-73.
- Payer M. Unstable burst fractures of the thoraco-lumbar junction: treatment by posterior bisegmental correction/fixation and staged anterior corpectomy and titanium cage implantation. Acta Neurochir (Wien). 2006;148(3):299-306;discussion 306.
- Ramani PS, Singhania BK, Murthy G. Combined anterior and posterior decompression and short segment fixation for unstable burst fractures in the dorso lumbar region. Neurol India. 2002;50(3):272-278.
- Suzuki T, Abe E, Miyakoshi N, et al. Anterior decompression and shortening reconstruction with a titanium mesh cage through a posterior approach alone for the treatment of lumbar burst fractures. Asian Spine J. 2012;6(2):123-130.
- Yang Z, Guo H, Gui S, Wang J, Ma X. [Anterior surgery for fourth lumbar burst fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2009;23(7):793-796.
- McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994;19(15):1741-1744.
- Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 4½-year series. Spine (Phila Pa 1976). 2000;25(9):1157-1170.
- Arand M, Kinzl L, Hartwig E. [Combined posterior and anterior endoscopic supported instrumentation of the thoracic and lumbar spine]. Arguments, concepts and first clinical results. Zentralbl Chir. 2002;127(6):490-496.
- Baulot E, Trouilloud P, Ragois P, Giroux EA, Grammont PM. [Anterior spinal fusion by thoracoscopy. A non-traumatic technique]. Rev Chir Orthop Reparatrice Appar Mot. 1997;83(3):203-209.
- Husson JL, Le Huec JC, Polard JL, Trebuchet G, Lesprit E, Bossis JM. [Interbody arthrodesis of the lumbar vertebrae using retroperitoneal videoendoscopy. A preliminary study of 38 cases]. Chirurgie. 1998;123(5):491-499.
- Kepler CK, Sharma AK, Huang RC. Lateral transpsoas interbody fusion (LTIF) with plate fixation and unilateral pedicle screws: a preliminary report. J Spinal Disord Tech. 2011;24(6):363-367.
- Kim DH, O'Toole JE, Ogden AT, et al. Minimally invasive posterolateral thoracic corpectomy: cadaveric feasibility study and report of four clinical cases. Neurosurgery. 2009;64(4):746-752;discussion 752-753.
- Kossmann T, Jacobi D, Trentz O. The use of a retractor system (SynFrame) for open, minimal invasive reconstruction of the anterior column of the thoracic and lumbar spine. Eur Spine J. 200;10(5):396-402.
- Payer M, Sottas C. Mini-open anterior approach for corpectomy in the thoracolumbar spine. Surg Neurol. 2008;69(1):25-31; discussion 31-2.
- Schnake KJ, Scholz M, Marx A, Hoffmann R, Kandziora F. Anterior, thoracoscopic-assisted reduction and stabilization of a thoracic burst fracture (T8) in a pregnant woman. Eur Spine J. 2011;20(8):1217-1221.
- Shawky A, Al-Sabrout AM, El-Meshtawy M, Hasan KM, Boehm H. Thoracoscopically assisted corpectomy and percutaneous transpedicular instrumentation in management of burst thoracic and thoracolumbar fractures. Eur Spine J. 2013;22(10):2211-2218.
- Spiegl UJ, Hauck S, Merkel P, Buhren V, Gonschorek O. [Incomplete cranial burst fracture in the thoracolumbar junction. Results 6 years after thoracoscopic monosegmental spondylodesis]. Unfallchirurg. 2014;117(8):703-709.
- Verheyden AP, Katscher S, Gonschorek O, Lill H, Josten C. [Endoscopically assisted minimally invasive reconstruction of the anterior thoracolumbar spine in prone position]. Unfallchirurg. 2002;105(10):873-880.
- Pimenta L. Lateral endoscopic transpsoas retroperitoneal approach for lumbar spine surgery. in VIII Brazilian Spine Society Meeting. Belo Horizonte, Minas Gerais Brazil. 2001.
- Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006;6(4):435-443.
- Cloward RB. Lumbar intervertebral disc surgery; description of a new instrument, the vertebra spreader. Surgery. 1952;32(5):852-857.
- Lin PM. A technical modification of Cloward's posterior lumbar interbody fusion. Neurosurgery. 1977;1(2):118-124.
- Herrera AJ, Berry CA, Rao RD. Single-level transforaminal interbody fusion for traumatic lumbosacral fracture-dislocation: a case report. Acta Orthop Belg. 2013;79(1):117-122.
- Schmid R, Krappinger D, Blauth M, Kathrein A. Mid-term results of PLIF/TLIF in trauma. Eur Spine J. 2011;20(3):395-402.
- Wang L, Li J, Wang H, et al. Posterior short segment pedicle screw fixation and TLIF for the treatment of unstable thoracolumbar/lumbar fracture. BMC Musculoskelet Disord. 2014;15;40.
- Harms J, Jeszenszky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998;6(2):88-99.
- Resnick DK, Benzel EC. Lateral extracavitary approach for thoracic and thoracolumbar spine trauma: operative complications. Neurosurgery. 1998;43(4):796-802.
- Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disorders Tech. 2005;18:S1-S6.
- Been HD, Bouma GJ. Comparison of two types of surgery for thoraco-lumbar burst fractures: combined anterior and posterior stabilisation vs. posterior instrumentation only. Acta Neurochir (Wein). 1999;141(4):349-357.
- Daniaux H, Seykora P, Genelin A, Lang T, Kathrein A. Application of posterior plating and modifications in thoracolumbar spine injuries. Indication, techniques, and results. Spine (Phila Pa 1976). 1991;16(3):S125-S133.
- Dickman CA, Yahiro MA, Lu H, Melkerson MN. Surgical treatment alternatives for fixation of unstable fractures of the thoracic and lumbar spine. A meta-analysis. Spine (Phila Pa 1976). 1994;19(20):2266S-2273S.
- Haiyun Y, Rui G, Shucai D, et al. Three-column reconstruction through single posterior approach for the treatment of unstable thoracolumbar fracture. Spine (Phila Pa 1976). 2010;35(8):E295-E302.
- Knop C, Kranabetter T, Reinhold M, Blauth M. Combined posterior–anterior stabilisation of thoracolumbar injuries utilising a vertebral body replacing implant. Eur Spine J. 2009;18(7):949-963.
- Reinhold M, Knop C, Beisse R, et al. [Operative treatment of traumatic fractures of the thoracic and lumbar spinal column: Part III: Follow up data]. Unfallchirurg. 2009;112(3):294-316.
- Resch H, Rabl M, Klampfer H, Ritter E, Povacz P. [Surgical vs. conservative treatment of fractures of the thoracolumbar transition]. Unfallchirurg. 2000;103(4):281-288.
- Vaccaro AR, Lim MN, Hurlbert RJ, et al. Surgical decision making for unstable thoracolumbar spine injuries: results of a consensus panel review by the Spine Trauma Study Group. J Spinal Disord Tech. 2006;19(1):1-10.
- Carl AL, Tranmer BI, Sachs BL. Anterolateral dynamized instrumentation and fusion for unstable thoracolumbar and lumbar burst fractures. Spine (Phila Pa 1976). 1997;22(6):686-690.
- Esses SI, Botsford DJ, Kostuik JP. Evaluation of surgical treatment for burst fractures. Spine (Phila Pa 1976). 1990;15(7):667-673.
- Schnee CL, Ansell LV. Selection criteria and outcome of operative approaches for thoracolumbar burst fractures with and without neurological deficit. Journal of neurosurgery. 1997;86(1):48-55.
- van Loon JL, Slot GH, Pavlov PW. Anterior instrumentation of the spine in thoracic and thoracolumbar fractures: the single rod versus the double rod Slot-Zielke device. Spine (Phila Pa 1976). 1996;21(6):734-740.
- Aebi M, Etter C, Kehl T, Thalgott J. The internal skeletal fixation system a new treatment of thoracolumbar fractures and other spinal disorders. Clin Orthop Relat Res. 1988;227:30-43.
- Jaffray DC, Eisenstein S, Balain B, Trivedi JM, Newton Ede M. Early mobilisation of thoracolumbar burst fractures without neurology: a natural history observation. Bone Joint J. 2016;98-B(1):97-101.
- McLain RF. Functional outcomes after surgery for spinal fractures: return to work and activity. Spine (Phila Pa). 2004;29(4):470-477.
- Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976). 2001;26(9):1038-1045.
- Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005;18(6):485-488.
- Wild MH, Glees M, Plieschnegger C, Wenda K. Five-year follow-up examination after purely minimally invasive posterior stabilization of thoracolumbar fractures: a comparison of minimally invasive percutaneously and conventionally open treated patients. Arch Orthop Trauma Surg. 2007;127(5):335-343.
- Knop C, Blauth M. [Bisegmental stability and Synex.] Unfallchirurg. 2003;106(3):259-261.
- Lange U, Edeling S, Knop C, Bastian L, Krettek C, Blauth M. [Titanium vertebral body replacement of adjustable size. A prospective clinical trial]. Unfallchirurg. 2006;109(9):733-742.
- Whitesides TE Jr. Traumatic kyphosis of the thoracolumbar spine. Clin Ortho and Relat Res. 1977;128:78-92.
- Schmid R, Krappinger D, Seykora P, Bauth M, Kathrein A. PLIF in thoracolumbar trauma: technique and radiological results. Eur Spine J. 2010;19(7):1079-1086.
- Farcy JP, Glassman SD. Sagittal index in management of thoracolumbar burst fractures. Spine (Phila Pa 1976). 1990;15(9):958-965.
- Neumann P, Nordwall A, Osvalder A. Traumatic instability of the lumbar spine. A dynamic in vitro study of flexion-distraction injury. Spine (Phila Pa). 1995;20(10):1111-1120.
- Daffner RH, Deeb ZL, Goldberg AL, Kandabarow A, Rothfus WE. The radiologic assessment of post-traumatic vertebral stability. Skeletal Radiol. 1990;19(2):103-108.
- Schnake K, Von Scotti F, Haas N, Kandziora F. Typ-B-Distraktionsverletzungen der thorakolumbalen Wirbelsäule. Der Unfallchirurg. 2008;111(12):977-984.
- Bühren V, Josten C. Chirurgie der verletzten wirbelsäule: frakturen, instabilitäten, deformitäten. 2012: Springer-Verlag.
- Schreiber U, Bence T, Grupp T, et al. Is a single anterolateral screw-plate fixation sufficient for the treatment of spinal fractures in the thoracolumbar junction? A biomechanical in vitro investigation. Eur Spine J. 2005;14(2):197-204.
- Wilke HJ, Kemmerich V, Claes LE, Arand M. Combined anteroposterior spinal fixation provides superior stabilisation to a single anterior or posterior procedure. J Bone Joint Surg Br. 2001;83(4):609-617.
- Domenicucci M, Preite R, Ramieri A, Ciappetta P, Delfini R, Romanini L. Thoracolumbar fractures without neurosurgical involvement: surgical or conservative treatment? J Neurosurgical Sci. 1996;40(1):1-10.
- Knop C, Fabian HF, Bastian L, Blauth M. Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine (Phila Pa 1976). 2001;26(1):88-99.
- Panjabi MM, Oxland TR, Kifune M, Arand M, Wen L, Chen A. Validity of the three-column theory of thoracolumbar fractures. A biomechanic investigation. Spine (Phila Pa 1976). 1995;20(10):1122-1127.
- Panjabi MM, Oxland TR, Lin RM, McGowen TW. Thoracolumbar burst fracture. A biomechanical investigation of its multidirectional flexibility. Spine (Phila Pa 1976). 1994;19(5):578-585.
- Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976). 2001;26(5):567-571.
- Daniaux H. [Transpedicular repositioning and spongioplasty in fractures of the vertebral bodies of the lower thoracic and lumbar spine]. Unfallchirurg. 1986;89(5):197.
- De Iure F, Cappuccio M, Paderni S, Bosco G, Amendola L. Minimal invasive percutaneous fixation of thoracic and lumbar spine fractures. Minim Invasive Surg. 2012;2012:141032.
- Schmidt OI, Strasser S, Kaufmann V, Strasser E, Gahr RH. Role of early minimal-invasive spine fixation in acute thoracic and lumbar spine trauma. Indian J Orthop. 2007;41(4):374-380.
- Tinelli M, Matschke S, Adams M, Grutzner PA, Munzberg M, Suda AJ. Correct positioning of pedicle screws with a percutaneous minimal invasive system in spine trauma. Orthop Traumatol Surg Res. 2014;100(4):389-393.
- Oh CH, Ji GY, Jeon JK, Lee J, Yoon SH, Hyun DK. Slip reduction rate between minimal invasive and conventional unilateral transforaminal interbody fusion in patients with low-grade isthmic spondylolisthesis. Korean J Spine. 2013;10(4):232-236.
- Rouben D, Casnellie M, Ferguson M. Long-term durability of minimal invasive posterior transforaminal lumbar interbody fusion: a clinical and radiographic follow-up. J Spinal Disord Tech. 2011;24(5):288-296.
- Zairi F, Allaoui M, Thines L, Arikat A, Assaker R. [Transforaminal lumbar interbody fusion: goals of the minimal invasive approach]. Neurochirurgie. 2013;59(4-5):171-177.
- Capener N. The evolution of lateral rhachotomy. J Bone Joint Surg Br. 1954;36(2):173-179.
- Larson SJ, Holst RA, Hemmy DC, Sances A Jr. Lateral extracavitary approach to traumatic lesions of the thoracic and lumbar spine. J Neurosurgery. 1976;45(6):628-637.
- Delfini R, Di Lorenzo N, Ciappetta P, Bristot R, Cantore G. Surgical treatment of thoracic disc herniation: a reappraisal of Larson's lateral extracavitary approach. Surg Neurol. 1996;45(6):517-522.
- Browner BD, Jupiter JB, Krettek C, Anderson PA. Skeletal Trauma: Basic Science, Management, and Reconstruction. Elsevier Health Science; 2009.
- Vaccaro A, Kandziora F, Fehlings M, Shanmughanathan M. Thoracic and lumbar Trauma. AO Foundation. 2014;
https://www2.aofoundation.org/wps/portal/surgery?showPage=diagnosis&bone=Spine&segment=TraumaThoracolumbar. Accessed April3, 2019. - Beisse R. Endoscopic surgery on the thoracolumbar junction of the spine. Eur Spine J. 2006;15(6):687-704.
- Danisa OA, Shaffrey CI, Jane JA, et al. Surgical approaches for the correction of unstable thoracolumbar burst fractures: a retrospective analysis of treatment outcomes. J Neurosurg. 1995;83(6):977-983.
- Fraser RD. Interbody, posterior, and combined lumbar fusions. Spine (Phila Pa 1976).1995;20:167S-177S.
- Ray CD. Threaded titanium cages for lumbar interbody fusions. Spine (Phila Pa 1976). 1997;22(6):667-679.
- Faciszewski T, Winter RB, Lonstein JE, Denis F, Johnson L. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine (Phila Pa 1976). 1995;20(14):1592-1599.
- Baker JK, Reardon PR, Reardon MJ, Heggeness MH. Vascular injury in anterior lumbar surgery. Spine (Phila Pa 1976).1993;18(15):2227-2230.
- Jacobs M, Verdeja J, Goldstein H. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1(3):144-150.
- Bergey DL, Villavicencio AT, Goldstein T, Regan JJ. Endoscopic lateral transpsoas approach to the lumbar spine. Spine (Phila Pa 1976). 2004;29(15):1681-1688.
- Nakamura H, Ishikawa T, Konishi S, Seki M, Yamano Y. Psoas strapping technique: a new technique for laparoscopic anterior lumbar interbody fusion. J Am Coll Surg. 2000;191(6):686-688.
- Christensen FB, Bünger CE. Retrograde ejaculation after retroperitoneal lower lumbar interbody fusion. Int Orthop. 1997;21(3):176-180.
- Zdeblick TA, David SM. A prospective comparison of surgical approach for anterior L4–L5 fusion: laparoscopic versus mini anterior lumbar interbody fusion. Spine (Phila Pa 1976). 2000;25(20):2682-2687.

