- See:
- Facet Joint Injuries
- Hyperflexion Injuries
- Oblique projections;
- Pillar View
- Discussion:
- simple unilateral facet dislocation is often a stable injury, eventhough there is disruption of the posterior ligament complex (involved
joint capsule, posterior longitudinal ligament, and annulus);
- mechanism & anatomy of injury:
- injury involves forward rotation of one side of vertebra about contra-lateral facet joint;
- simultaneous flexion-rotation injury produces unilateral interfacetal dislocation;
- interfacetal joint on side of direction of rotation is pivot:
- superior facet on contralateral side rides upward, forward,& over tip of inferior facet of involved joint, coming to rest in intervertebral
foramen anterior to inferior facet of joint;
- in this position, the intervertebral forament is "locked;"
- central portion of vertebral body subluxates about 25% of AP body diameter;
- associated injuries:
- inferior facet of dislocated joint is frequently treated;
- capsule of non dislocated joint is frequently disrupted;
- facet dislocations can also occur w/ concomitant frx of either facet or the entire lateral mass;
- partial tearing of posterior longitudinal ligament on affected side(s);
- anterior longitudinal ligament remains intact;
- Clinical Manifestation:
- physical exam of the cervical spine:
- delays in diagnosis are not rare (40% of patients in one study).
- pts may have torticollis:
- axial rotation to contralat side & lateral bend to injured side.
- Radiographs:
- AP View:
- involved spinous process points to involved side;
- lateral view:
- mild anterior subluxation of vertebral body above &soft-tissue swelling anteriorly;
- vertebral body is anteriorly displaced ( < 50% AP diameter)
- decrease overlap of articular processes relative to facet joint above;
- two lateral masses of dislocated vertebra will overlap only partially on lateral view producing"bow tie" sign;
- oblique view:
- anteriorly dislocated inferior articular process is forced down into lower 1/2 of neuroforamen, causing nerve root compression;
- may readily be seen on the trauma oblique radiograph.
- dynamic lateral radiographs:
- (physician supervised) may determine if there is hypermobility;
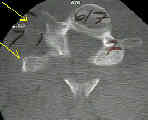
- tomography:
- is useful to determine presence of a frx & extent of displacement;
- MRI:
- disk herniation can be identified either by MRI or by myelography;
- anterior diskectomy and interbody fusion may be necessary if significant disk extrusion is present;
- failure to recognize a significant disk extrusion, which more commonly occurs with bilateral facet dislocation, can result in a catastrophic
neurologic deficit;
- Reduction:
- Non Operative Treatment:
- management of the spine injured patient:
- minimal subluxation is treated w/ Philadelphia-type collar for 6 wks;
- need careful f/u to ensure progressive subluxation does not occur;
- w/o disk widening or subluxation, unilateral facet dislocation is stable injury;
- if there is < 3.5 mm of translation assoc w/ this frx-dislocation, spine can undergo attempted reduction & halo immobilization;
- first try skeletal traction, followed by open reduction if unsuccessful.
- use of closed reduction by manipulation under GEA should be used only w/ flouroscopy:
- successful closed reduction is followed either by halovest (for 3 month), or by posterior wiring & bone grafting.
- closed reduction w/ halo traction is successful in 50 % of pts;
- these may be treated with halo vest immobilization;
- Indications for Surgery:
- failed closed reduction:
- if flexion extension views demonstrate persistent instability after 12 weeks, posterior stabilization is indicated;
- middle column injury
- this injury frequently leads to late instability;
- early single level posterior fusion is therefore recommended;
- signs of middle column disruption
- unilateral facet dislocation accompanied by > 25% subluxation;
- greater than 1.7 mm of disk widening;
- if initial displacement is > 3.5 mm;
- angulation > 11 deg (more than adjacent segments)
- Posterior Approach:
- open reduction is generally performed posteriorly, which allows direct visualization of the articular processes;
- posterior wiring w/ ICBG is performed for progressive subluxation;
- internal fixation must neutralize rotational forces;
- facet wiring & lateral mass plating may be used;
- w/ articular process frx or floating lateral mass bony block then resisting anterior shift on affected side may be lost, & additional
fixation is needed;
- Anterior Approach:
- provides a limited view & further disrupts disk;
- allows complete removal of disk, which eliminates risk of inducing paralysis from disk extrusion during reduction
- Case Example:



Closed reduction of cervical spine dislocations.
Unilateral facet dislocations and fracture-dislocations of the cervical spine.

