- See: Anatomy of C1 / C2
- Discussion:
- classically described as a 4 part burst frx of the atlas, w/ combined anterior and posterior arch fractures;
- frx variants: include two and three part fractures;
- pediatric frx:
- frx proceeds thru open synchondroses, and may occur w/ minimal trauma;
- posterior synchondroses fuses at age 4;
- anterior synchondroses fuses at age 7;
- mechanism:
- original description in 1920 noted role of axial compression;
- may also be caused by hyperextension, causing a posterior arch fracture;
- associated injuries:
- approx 1/3 of these fractures are associated with a axis fracture;
- approx 50% chance that some other C-spine injury is present;
- low rate of neurologic deficits is due to large breadth of C1 canal;
- Exam:
- pts usually complain of upper neck pain;
- pts are usually neurologically intact;
- in cases of vertebral artery injury, neurologic injury can occur;
- neurologic injury may manifiest as Wallenberg's syndrome w/ ipsilateral loss of cranial nerves,Horner's syndrome, ataxia, and
loss of contra-lateral pain and temp. sensation;
- Radiographs:

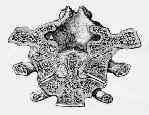
- Odontoid view:
- open mouth odontoid view shows overlapping of C1 facets on C2 facets;
- if sum of lateral mass displacement over articularsurfaces of axis is > 7 mm, transverse ligamentis likely
to be torn;
- this fracture is therefore considered unstable & should be rx'ed in halo for 3 months;
- children:
- overlapping lateral masses can be a normal variant in children and therefore this view may not allow assessment of whether frx is
stable or unstable;
- Lateral view:
- shows prevertebral soft tissue widening
- if atlantodental interval is > 4 mm, there may be a rupture of the transverse ligament;
- if antantal dens interval is > 6 mm, transverse ligament is presummed to be disrupted and the injury is unstable;
- fusion anomalies of theAtlas differ from a burst frx in that fusion defect has well corticated margins and is associated w/ no soft
tissue swelling;
- Flexion and Extension Views:
- usually required to determine whether there is transverse ligament disruption;
- atlantodens interval > 3 mm indicates hypermobility;
- may detect concomitant anterior hypermobility;

- CT Scan:
- probably should be ordered for all children suspected of having Jefferson frx, since the odontoid view may be difficult to interpret;
- additional information may be provided by a CT scan, which may detect ligament avulsion frx, even if displacement is < 7 mm;
- CT of C1 is often helpful in further delineating exact displacement of fragments;
- Treatment of Stable Frx:
- by definition stable fractures are those w/ intact transverse ligament;
- nondisplaced or minimally displaced frx is rx'ed w/ orthosis;
- soft-collar treatment is sufficient for isolated posterior arch frx;
- w/ minimally displaced fracture (and overhang is < 7 mm), then frx is stable and should be treated in a rigid support, such as a
cervicothoracic brace, for 3 month;
- although late subluxation of C-1 is not common, it should be looked for following bony healing;
- Treatment of Unstable Frx:
- separation of lateral masses implies that transverse ligament is ruptured, and is therefore unstable;
- prolonged cranial traction is only method that will reduce lateral mass displacement, because halovest will not dependably produce
sustained traction;
- w/ adequate reduction following traction, halovest can be worn although late atlantoaxial instability may occur;
- halo or skeletal traction is necessary for a total of 3 months;
- w/ greater than 5 mm of C1-C2 subluxation consider C1-C3 fusion
References
Non-union of fractures of the atlas
Injuries of the atlas and axis. A follow-up study of 85 axis and 10 atlas fractures.

