- Discussion:
- occurs in children between ages of 6-10 yrs who sustain injury by falling on an outstretched hand;
- shearing forces of hyperextension & supination displace the distal radial epiphysis dorsally;
- great majority are Salter I and II:
- physeal frxs of of distal radius and ulna:
- w/ type I: look for anterior displacement of pronator quadratus fat pad;
- type II are usually displaced dorsally (account for about 60% of distal radius frx);
- type V frxs are impossible to dx until 6-12 months after time of injury (before obliteration of the physis is seen);
- prognosis:
- distal radial and ulnar physes provide 75-80% of total growth of forearm, so there is excellent potential for remodeling (correction of deformity);
- while distal radius physis is most frequently traumatically separated physis in the child, subsequent growth disturbance is unusual;
- Associated Injuries:
- in about one half of cases there will be a concomitant distal ulnar frx;
- may be assoc w/ green stick frx of metaphysis of ulna;
- there may also be separation of the distal ulnar epiphysis, or avulsion frx of the tip of the ulnar styloid process;
- non union of ulnar styloid after separation thru unossified styloid process becomes evident only after ossification occurs (usually by the end of 1st decade)
- occassionally causes symptoms with forearm rotation;
- Exam:
- soft tissue swelling can be impressive even in minimally displaced fractures;
- acute carpal tunnel syndrome is a reported complication;
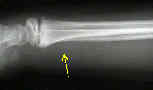
- Radiographs:
- lateral radiograph will best show posterior displacement of epiphysis;
- dorsal metaphyseal bone frag is small, requiring scrutiny for detection;
- hemorrhage into pronator quadratus fat pad will indicate amount of swelling;

- Reduction:
- w/ acute presentation closed reduction is usually easy;
- over reduction is difficult becuase of intact dorsal periosteum;
- if one or two attempts at closed reduction fail, consider leaving epiphysis displaced;
- Treatment:
- acceptable amount of displacement is not specifically known, however, 30% physeal displacement heals readily and 50% displacement may often completely remodel in 1.5 years;
- delayed presentation: (after 1-2 weeks)
- manipulation of fracture is not advised;
- repeated forceful manipulations are esp to to be avoided in SH I and II;
- forceful attempts at reduciton are likely to damage growth plate;
- distal radial physis has good remodeling potential which allows a displaced epiphysis to be left unreduced;
- w/ in 2 to 3 years, distal radial epiphysis will regain its normal relation to radial metaphysis;
- splint position:
- apply long arm splint w/ slight wrist flexion (25 deg) and ulnar deviation (15 deg), and with the arm in supination;
- initial casting is not advised with significant soft tissue swelling;
- splint is worn for 2 weeks, is then changed, & worn for 3 more wks;
- length of immobilization:
- immobilize in long arm cast for 3 to 4 weeks;
- Complications:
- compartment syndrome
- Compartmental syndrome complicating Salter-Harris type II distal radius fracture.
- growth plate arrest (see growth plate anatomy and physeal bone bridge)
- need to determine extent of the growth arrest;
- question is whether or not the arrest is resectable;
- CT scan will evaluate the extent of the growth arrest;
- if the arrest is not resectable then lengthening of the radius and epiphysiodesis of the ulna would adjust the appropriate length and alignment;
- references:
- Remodeling of Salter-Harris Type II Epiphyseal Plate Injury of the Distal Radius.
- Distraction Osteogenesis for Correction of Distal Radius Deformity After Physeal Arrest
- Growth and development of the distal radius and ulna
- Surgical management of posttraumatic distal radial growth arrest in adolescents.


