- Discussion:
- theory of tension band wiring:
- modified anterior tension band technique is indicated for both transverse and comminuted fractures of the patella;
- for maximal strength, wires are placed on tension surface of bone (anterior surface), as compared to circumferential cerclage wiring;
- frx fragments are opposed from tension of the figure of 8 wire passed thru insertions of the quadriceps tendon and patellar ligament;
- remember Sharpey's fibers provide the strongest site of fixation;
- two K wires or 4 mm cancellous lag scres are incorporated into figure of 8 wire to augment anchorage of cerclage wire;
- if there is too much comminution for secure ORIF, but a major (usually superior) fragment with a substantial amount of normal articular
cartilage is present, partial patellectomy is the appropriate approach;
- PreOp Planning:
- position patient supine w/ bump under knee;
- equipement: several large towel clamps, 14 gauge needle, 20 and 22 gauge wire, and K wires;
- be sure to explain to the patient that eventual hardware removal may be necessary due to pain;
- Incision:
- approached via a midline longitudinal incision or a transverse incision;
- transverse incision gives more cosmetic result, esp in young patients;
- be careful to avoid areas of contused skin or abrasions;
- soft tissue overlying patella is often injured from direct compression or abrasion at the time of the fracture;
- large frx hematoma frequently develops, further compromising soft tissues;
- Exposure:
- expose entire anterior surface of patella, and the quadriceps and patellar tendon;
- expose frx & identify any defect in the extensor mechanism;
- defects in retinaculum will extend several cm medially or laterally, or both;
- therefore extend exposure with a medial parapatellar capsular incision for a short distance proximally and medially.
- need enough release to allow adequate palpation & partial visualization of frx site to ensure anatomical reduction of the articular surface;
- look for osteochondral fragments, esp in trochlear groove;
- it is not necessary to create a large medial arthrotomy, such as would be necessary for eversion and full visualization of the articular
surface - small arthrotomy can be closed after fixation;
* before proceding, place simple sutures in the torn retinaculum on either side of the fracture, and clamp the suture ends (do not tie);
- the sutures are not tied at this point, becuase this would interfere w/ visualization of the fracture fragments;
- placing sutures across the torn retinaculum will facilitate their repair, after the fracture has been fixed;
- Reduction:
- integrity of the fragments is evaluated;
- often there is comminution that was not recognized on the radiographs;
- decision regarding whether to proceed with an ORIF, partial patellectomy, or total patellectomy is then re-evaluated;
- ORIF of transverse fractures with little or no comminution are most amenable to treatment with open reduction and internal fixation;
- two large towel clips may assist w/ the reduction;
- frx w/ small amount of comminution can often be first converted to a simple transverse frx by lag-screw fixation of comminuted portion;
- provisional stabilization of the fracture can usually be obtained with one or two bone-reduction forceps or with K wires;
- once articular reduction is assured, procede w/ hardware insertion;
- Tension Band Wiring w/ Cannulated Screws:
- main disadvantage is that there may be only a limited amount of bone to accomodate 2 cannulated screws;
- if hardware failure occurs, there may not be a good back up plan;
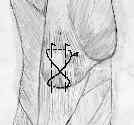
- K Wire Technique: (Modified Tension Band Technique);




- insert two parallel 2.0-millimeter smooth K wires from an inferior to superior direction (w/ ends left long to accomodate the tension band wire);
- K wires must be parallel for compression to take place;
- knee flexion is helpful during K wire insertion;
- alternatively, parallel longitudinal Kirschner wires can be inserted retrograde thru the frx site, which assures that the wires
will be inserted slightly anterior to the mid-point;
- it is important that the K wires be inserted slightly anteriorly in the patella in order for the tension band to function properly;
- further, posterior placement of K wires will leave the K wires deeply imbeded in the substance of the quadriceps and patellar tendons,
which will make future hardware removal difficult;
- attempt to insert the wires so that both wire tips are parallel to the anterior patellar surface (and therefore neither pin tip is excessively deep to the tendon surface);
- Passage of 18 gauge Wire:
- an 18-gauge wire is then passed across the anterior surface of the patella (either cross or not crossed) and passed directly behind the K wires;
- no soft tissue (quad or patellar tendon) should intervene between the the K wires or bone surface and the tensioned wire;
- hence, the tensioned wires are placed directly adjacent to the patellar surface and directly against the K wires;
- wire passage is facilitated w/ 14 gauge needle or angiocath;
- the wires will pass thru the anterior portions of the quadriceps and patellar tendons (just posterior to the K wires);
- circle configuration: arms of the wires are brought anteriorly over surface of patella, and each medial and lateral side is twisted and tightened;
- figure of 8 configuration: the wire is passed over the K wires in figure of eight configuration, anteriorly over the surface of the patella;
- note that wires placed in a figure of 8 fashion over the anterior patellar surface may end up causing excessive tenderness;
- consider using the standard circle configuration supplemented with the figure of 8 configuration, the later using a No 5 suture (to reduce tenderness);
- Twist and Cut the Wires:
- it is important to avoid having sharp protruding wires inferiorly as these can cause signficant pain or even lead to patellar tendon laceration;
- inferiorly, bend each end of the K wires 180 deg, cut short, and impact into the patellar bony surface;
- superiorly twist the K wires 180 degs and cut them short, but do not impact them (leaving the superior K wire tips slightly prominent will cause
less symptoms than leaving the inferior K wire tips prominent);
- cut the inferior protruding ends of the K wire short (3-4 mm from the bony surface so the K wires will not dislodge;
- some authors recommend, bending both the superior and inferior ends of the K wires inorder to prevent K wire migration;
- in the report by Wu CC, et al, the authors report 100% (62/62 fractures) and a union period of 2.5 ± 0.5 months;
- skin irritation was noted in 2 patients (3%)
- ref: Patellar tension band wiring: a revised technique
- Wound Closure:
- following hardware insertion, the extensor retinaculum is repaired;
- be sure to close the superficial retinaculum inorder to maximize coverage over the hardware;
- Post Operative Care:
- patient is immobilized for 2-3 weeks;
- begin prone hang exercises at 2-3 weeks;
- crutches are discontinued after 6 weeks
Patellar tension band wiring: a revised technique
Comparison of the mechanical properties of different tension band materials and suture techniques.
Experimental investigation of the tension band in fractures of the patella.