
- Discussion:
- primary internal fixation is treatment of choice for unstable scaphoid frxs;
- frx treated by primary internal fixation, avg time for return to work is 3.7 wks w/ union rate, 97 %;
- this compares very favorably with conservative treatment;
- indications for surgery:
- main indication is an unstable scaphoid frx as seen on x-ray or CT scan;
- displacment > 1 mm;
- radiolunate angle > 15 degrees;
- scapholunate > 60 degrees;
- implants:
- Herbert Screw
- 3.5 mm Cannulated Screw Insertion:
- relative fixation strength: (from Toby, et al (1997));
- volar comminution of the scaphoid is a major risk factor for hardware failure;
- AO screw, Acutrak screw, and the Herbert-Whipple screw have superior reistance to cyclic bending loads compared to the Herbert screw;
- A comparison of fixation screws for the scaphoid during application of cyclical bending loads.
- Anthropometry of the Human Scaphoid
- preoperative considerations:
- note that a dorsal humpback malunion is possible even with surgical fixation, and that even w/ small degrees of malunion will result in a significant loss of wrist extension;
- fracture is exposed using an anterior approach;
- w/ dislocation of the midcarpal joint, an attempt should be made to reduce this by closed manipulation before draping;
- if dislocation is unstable, or if there are signs of median nerve compression, a more extensive exposure is used:
- in complex frx-dislocations, it may be necessary to make dorsal as well as a volar approach to the carpus;
- flexor retinaculum is completely divided and the midcarpal joint approached through the floor of the carpal tunnel;
- outcomes of surgical treatment of scaphoid fracture
- Incision and Exposure: 


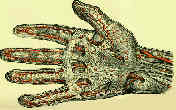
- tubercle of scaphoid is palpated distal to lower visible or palpable end of FCR;
- skin incision is centered over scaphoid tubercle and curved distally into thenar base;
- made proximally from tubercle for 3 cm, between tendon of FCR medially & radial artery laterally;
- incision is carried down between tendon of FCR & radial artery;
- radial artery & its palmar branch are on radial side of FCR;
- median nerve & its palmar branch are on ulnar side of the tendon;
- scaphoid is then approached thru separate longitudinal incision in capsule on radial side of FRC tendon;
- some surgeons prefer to longitudinally incise thru the dorsal bed of the FCR sheath;
- w/ acute frx, expect hemarthrosis in both the radiocarpal and the distal scaphoid joints, making the use of a fine sucker essential;
- distal scaphoid is exposed by making a transverse incision at the STT joint;
- alternate incision:
- may be indicate for extreme humpback deformities or radio-scaphoid impingement;
- consider using the interval between the radial artery and first extensor compartment (on the volar side) and the EPL (on the dorsal side);
- key to exposing the scaphoid lies in dorsiflexion of wrist and axial traction on the thumb;
- this will expose the proximal pole of scaphoid, which is site of most cases of nonunion;
- avoid dividing the the radioscaphoid capitate ligament;
- preservation of the radioscaphoid ligament maintains the proximal pole of the scaphoid in a reduced position in the fossa of the distal part of the radius;
- w/ division of the radioscaphoid ligament is divided, the proximal pole may translate in a volar direction, complicating the reduction;
- Debridment:
- in cases of non-union use curets or highspeed burr to debride the non union site of fibrous tissue, while taking care not to damage the outer cortical shell;
- alternatively consider using a 3 mm oscillating saw inorder to cut the scaphoid back to bleeding bone;
- Reduction:
- consider using dental picks to manipulate the frx fragments into reduction;
- K wires can be inserted perpendicular to the frx fragments inorder to "joystick" them into reduction, but this may cause further comminution;
- in cases of scaphoid humback deformity the lunate should be reduced before correcting the scaphoid deformity;
- the lunate should be reduced back to a neutral position by pinning it to the radius;
- note that even a small humpback deformity will leave the patient with restricted dorsiflexion;
- if the reduction is difficult, articular border of the scaphoid with the capitate can be used as a "mold" inorder to realign the fractured scaphoid;
- Guide Wire Insertion:
- the key to proper guide wire insertion is good visualization of the scaphoid;
- insert a freer elevator along the proximal-radial aspect of the scaphoid (into the radial-carpal joint), inorder to allow a lateral view of the scaphoid;
- in many cases, the guide wire will be inserted too volarly and is not directed adequately to the distal-ulnar tip of the scaphoid;
- consider using a rongeur to remove a small portion of the non articulating portion of the trapezium inorder to allow a more dorsal insertion of the guide wire;
- A Comparison of 2 Methods for Scaphoid Central Screw Placement From a Volar Approach
- stabilizing guide wire:
- place a guide wire along the radial border of the scaphoid to control rotation;
- once this guide wire is in place, wrist can be ulnarly deviated to better expose the scaphoid body for wire insertion down the central third of proximal pole;
- Trumble, et al (1996), left the second stabilizing K wire in place for 6-8 weeks postop;
- cannulated screw guide wire:
- as pointed out by Trumble, et al (1996), the key to a successful result is placement of the guide wire in the central third of the proximal pole of the scaphoid;
- these authors emphasized that the guide wire needs to be placed in the central third of the proximal scaphoid on both PA, lateral, and oblique radiographs;
- Non-union of the scaphoid. Treatment with cannulated screws compared with treatment with Herbert screws.
- Pronated Oblique View in Assessing Proximal Scaphoid Articular Cannulated Screw Penetration
- Wound Closure:
- when performing a volar approach, radioscaphocapitate ligament and palmar radiolunate-triquetral ligament must be partially or totally divided;
- see ligaments of the wrist;
- if inadequately repaired, the natural tendency of the lunate to extend and the scaphoid to flex under axial compression may lead to a DISI deformity;
- Post Op Care:
- even w/ ORIF many recommend that immobilization be continued in short thumb-spica cast until there is evidence of frx union;
- note that with cannulated screw fixation, average time to union is about 4 months
Dorsal approach to scaphoid nonunion.
Corrective osteotomy for scaphoid malunion: technique and long-term follow-up evaluation.
The Herbert screw for scaphoid fractures. A multicentre study.
Scaphoid fractures: dorsal versus volar approach.
Operative management of pediatric scaphoid fracture nonunion.



















