- Discussion:
- indicated for SI joint disruptions and for some sacral fractures;
- Operative Technique:
- radiographs:
- surgical stratedgy:
- if anterior pelvic injury:
- note that the biggest risk factor for postoperative SI joint displacement is failure to recognize and treat anterior pelvic injury;
- fixation failure rates are much higher when iliosacral screws are combined with anterior pelvic external fixation devices;
- in contrast, iliosacral screw fixation is useful for combined anterior/posterior injuries when percutaneous SI joint screw
fixation is augmented by rigid anterior fixation;
- if the patient is to be placed in the prone position (for SI fixation), then the anterior lesion needs to be fixed with a plate
(rather than an external fixator);
- if an extenal fixator is to be used, then the patient will have to undergo posterior fixation in the supine position (if the
fixator is to be applied first), otherwise iliosacral screws must be inserted first (prone position) and then patient is
turned for application of fixator;
- likewise concomitant acetabular frx should be fixed first;
- once posterior reduction is achieved, fixation of joint dislocation is done via lag screws placed across joint from ilium to sacral
ala lateral to the sacral body, avoiding nerves;
- managed in a fashion similar to that used for sacral fracture;
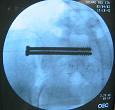
- screws are directed across SI joint into the sacral ala, into the body of S1;
- often screws need to be passed across the midline inorder to achieve adequate fixation;
- when poor screw purchase is achieved, a second screw is inserted inorder to lock threads with the first screw;
- in some cases, screws are directed into the body of S2;
- patients can be placed in the supine, prone position, or lateral position;
- supine positioning allows easier closed reduction of the hemipelvis, and when SI joint dislocations cannot be reduced
closed, supine position allows open reduction and anterior SI joint fixation;
- ref: Early Results of Percutaneous Iliosacral Screws Placed with the Patient in the Supine Position.
- screws can be inserted thru percutaneous incisions thru the buttocks muscle, regardless of the condition of the local soft tissues;
- percutaneous technique is less likely to cause infection when a degloving injury is present;
- methods to decrease complications:
- surgeon's finger is passed thru the greater sciatic notch to protect anterior structures;

- Flourscopic Imaging:
- note that high quality floursoscopic equipment is required for screw placement, noting that in the series by
Keating, et al (1999) there were two patients that had screws protruding through the S1 foramen that was
only apparent on the postop radiographs;
- ref: Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion.
- may be performed in the supine or prone position;
- typically the supine position is used if the procedure is to be performed using a percutaneous
technique (and in this case it is important that it be confirmed that a closed reduction be
obtainable before the surgeon commits to this technique);
- note: adequate reduction is manditory prior to screw insertion;
- w/o reduction, left and right anterior iliac cortical densities as well as the greater sciatic notches cannot be superimposed;
- most common target on sacrum is body of first sacral segment, and it may not be necessary for the screw to engage the far SI joint;
- ref: The Effect of Transiliac-Transsacral Screw Fixation for Pelvic Ring Injuries on the Uninjured Sacroiliac Joint.
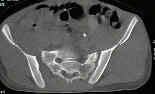
- SI joint anatomy: SI joint has an L shaped configuration;
- one limb runs about 1 cm above the inferior border of the iliac wing;
- second limb runs almost vertically for about 3 cm in length, and is positioned about 4 cm from the PIIS and
about 5.5 cm from PSIS;
- reference:
- The Location of the Sacroiliac Joint on the Outer Table of the Posterior Ilium.
- outlet view is used to direct the guide pin tip cephalad to the sacral nerve foramen;
- need to identify the curvilenear iliac cortical density which parallels the anterior aspect of the SI joint;
- the safe zone lies between the alar cortex supero-anteriorly and the sacral neural foramen posteriorly;
- using inlet and outlet views, guide pins are inserted upto a point lateral to the ipsilateral S1 neural foramen;
- lateral view of sacrum helps direct the guide pin tip caudal to the ICD and then into the sacral ala;
- once the lateral view confirms that the pin is optimally placed, the pin can be driven to the midline;
- references:
- Is the lateral sacral fluoroscopic view essential for accurate percutaneous sacroiliac screw insertion? An experimental study.
- Transsacral versus modified pelvic landmarks for percutaneous iliosacral screw placement--a computed tomographic analysis and cadaveric study.
- Percutaneous placement of iliosacral screws for unstable pelvic ring: comparison between one and two C-arm techniques.
- Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study.
- Are two different projections of the inlet view necessary for the percutaneous placement of iliosacral screws?
- reduction methods:
- Intraoperative use of the pelvic c-clamp as an aid in reduction for posterior sacroiliac fixation.
- case examples:




- Structures at Risk:
- posteriorly the cauda equina;
- anteriorly ureter & elements of lumbosacral plexus & some branches of bifurcation of the common iliac artery;
- superiorly, the L5-S1 disk and the L5 nerve root;
- inferiorly the S1 nerve root
- if screw is aimed too low and crosses the S1 foramenae;
- superior gluteal artery:
- Superior Gluteal Artery Injury During Iliosacral Screw Placement due to Aberrant Anatomy
- Complications:
- S1 nerve root injury (may occur despite high quality flourscopic images);
- deep infection (more common w/ the Morel Lavel lesion);
- acute malreduction: upto 15% of patients will have a malreduction on immediate postoperative films;
- loss of fixation: up to 25% of patients will experience loss of reduction during the first postoperative month;
- patients at risk for displacement include those with recognized anterior injuries that did not receive anterior plating or external
fixation;
- Biomechanical Concepts for Fracture Fixation.
- pain:
- note that the majority of patients (85%) will have chronic SI joint pain, and 10% of patients may ultimately require SI joint
fusion (due to pain)
- references:
- Superior Gluteal Artery Injury During Iliosacral Screw Placement due to Aberrant Anatomy
- Inadvertent intraforaminal iliosacral screw placement despite apparent appropriate positioning on intraoperative fluoroscopy.
- Risks to the Superior Gluteal Neurovascular Bundle During Percutaneous Iliosacral Screw Insertion: An Anatomical Cadaver Study.
- Superior gluteal artery injury during iliosacral screw placement.
- The incidence of and factors affecting iliosacral screw loosening in pelvic ring injury
- The effect of sacral fracture malreduction on the safe placement of iliosacral screws.
- Biomechanical Comparison of Sacroiliac Screw Techniques for Unstable Pelvic Ring Fractures.
- Percutaneous iliosacral screw fixation: early treatment for unstable posterior pelvic ring disruptions.
- Useful Intraoperative Technique for Percutaneous Stabilization of Bilateral Posterior Pelvic Ring Injuries
- Case Example:
Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion.
The effect of sacral fracture malreduction on the safe placement of iliosacral screws.
Biomechanical Comparison of Sacroiliac Screw Techniques for Unstable Pelvic Ring Fractures.
The lateral sacral triangle--a decision support for secure transverse sacroiliac screw insertion.
The antishock iliosacral screw.
Transiliac-transsacral screws for posterior pelvic stabilization.
Vertically Unstable Pelvic Fractures Fixed with Percutaneous Iliosacral Screws: Does Posterior Injury Pattern Predict Fixation Failure?
S2 iliosacral screw fixation for disruptions of the posterior pelvic ring: a report of 49 cases.
An anatomic study on the placement of the second sacral screw and its clinical applications
The effect of sacral fracture malreduction on the safe placement of iliosacral screws.
Early Results of Percutaneous Iliosacral Screws Placed with the Patient in the Supine Position.
Biomechanical Comparison of Sacroiliac Screw Techniques for Unstable Pelvic Ring Fractures.