- Equipment:
- one or two appropriately sized reduction tenaculi;
- one sharp awl;
- either the cannulated 4.0 drill set or the small fragment set with two 2.5 mm drills (for 4.0 mm cancellous bone screws);

- Incision:
- curvilinear incision over medial malleolus;
- proximal portion of incision is centered over mid tibia, to allow adequate space for reduction tenaculum;
- distal portion of the incision is curved anteriorly, in order to allow space for the drill bits which usually must be angled slightly posteriorly;
- hazards:
- anteriorly be aware of the saphenous vein;
- posteriorly be awre of the tibialis posterior;
- Fracture Exposure:
- periosteum is elevated off the fracture site along the entire distance of the fracture;
- it is especially important to achieve anterior and posterior visualization;
- look for posterior medial cortical comminution;
- it is not necessary to strip the periosteum off the distal fragment;
- soft tissue is grasped over deltoid ligament w/ bone tenaculum & distracted allowing visualization thru internal aspect of joint;
- alternatively a bone hook can be used to pull the distral fragment distally allowing expsure of the ankle joint;
- joint space is copiously irrigated and loose bodies are identified;
- look for osteochondral lesions;
- Frx Reduction:
- using a 2 mm drill bit, drill a hole thru the tibial cortex 2-3 cm above the frx site;
- place an appropriately size tenaculum over the frx site, w/ one tip placed into the superior drill hole, and the other tip placed precisely over the center of the distal frx fragment;
- a sharp awl can be used to facilitate the frx reduction as the tenaculum is closed shut;
- ensure that an anatomic reduction has been achieved along both the anterior and posterior cortices;
- Preparation for Hardware Insertion:
- use marking pen to mark the anterior and posterior limits of the tibia;
- note how the fracture is angled posteriorly;
- it is important for the screws to be placed parallel to one another as well as perpendicular to the frx site, (but they should not be angled too posteriorly since this will cause the more posterior screw to hit the posterior cortex;
- the screw need to be inserted thru distal (inferior) surface of medial malleolus;
- this requires judicious dissection w/ the cautery to mark out two optimal screw insertion sites;
 - note that insertion of the screws thru inferior surface of medial malleolus makes it more likely that guide wires might be inserted into the ankle joint;
- note that insertion of the screws thru inferior surface of medial malleolus makes it more likely that guide wires might be inserted into the ankle joint;
- articular penetration is avoided by keep the guide wire positioned almost parallel to the tibia;
- in addition the screw heads will be directly over the tibialis posterior;
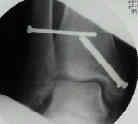
- Cannulated Technique: (for 4.0 mm screws)
- insert one threaded guide wire anterior to the tenaculum and one guide wire posterior to the tenaculum;
- again take care not to angle the screws too posteriorly;
- insert the guide wires a distance of about 5 cm;
- insert 2.7 mm drill bit over each guide wire and drill across the fracturesite (further drilling risks transection of the guide wires);
- two 40 to 50 mm 4.0 cannulated cancellous screws are advanced;
- once the screws cross the frx site, remove both guide pins (again to avoid transection of the wires);
- screw threads should gain purchase only in distal metaphysis about 2 to 4 cm above the joint, where densest cancellous bone is present;
- it is not necessary to engage opposite cortex unless there is osteoporosis;
- AP and lateral x-rays are obtained to confirm fracture reduction.
------------------------------------------



------------------------------------------------
Comparison of Surgical Techniques of 111 Medial Malleolar Fractures Classified by Fracture Geometry.




