Cervical Radiculopathy: Diagnosis and Treatment
Richard J. Nasca, MD
Nasca RJ. Cervical radiculopathy: current diagnostic and treatment options. J Surg Orthop Adv. 2009;18(1):13-18.
Introduction:
- Pain around the shoulder, arm and hand may be caused by irritation or compression of one or more cervical nerve roots.
- In the majority of patients, the symptoms are of short duration and resolve without treatment.
- If the root is irritated and not compressed, radiculitis results. Radiculopathy occurs when the root is compressed or involved with an intrinsic disease.
- Objective neural deficits, namely motor, sensory and reflex changes are seen with radiculopathy, whereas they are not found with radiculitis.
Natural History:
- Degenerative disc disease starts in the third decade of life with the loss of notochord cells and changes in the collagen and proteoglycan content of the disc.
- There is less hydration of the nucleus. Annular fissures occur followed by a loss of intradiscal contents and formation of osteophytes which may result in nerve root compression. (Fig 1.)
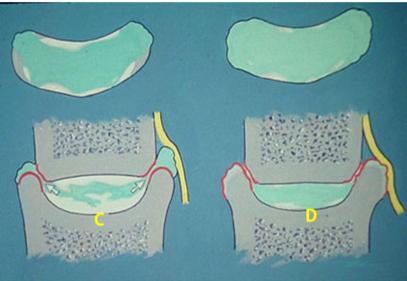
Fig 1. A, normal disc. B, Degenerating disc with annular fissures. C, Degenerating disc with herniation and nerve root compression. D, Degenerative disc, Luschka joint osteophytes and nerve root compression.
Used with the permission of the Southern Orthopaedic Association. Nasca RJ. Cervical radiculopathy: current diagnostic and treatment options. J Surg Orthop Adv. 2009;18(1):13-18.
- There is less hydration of the nucleus. Annular fissures occur followed by a loss of intradiscal contents and formation of osteophytes which may result in nerve root compression. (Fig 1.)
- The disc may become mechanically unsound and provide less stability. The adjacent bone attempts to stabilize the disc-vertebral body complex with osteophytes. As the disc degenerates, the nerve root canals become smaller in diameter and facet and Luschka joint osteophytes result in further compromise of the neural foramen. (Fig 2.)
Fig 2. Artist drawing of a cervical nerve root surrounded by foraminal and Luschka joint osteophytes.
Used with the permission of the Southern Orthopaedic Association. Nasca RJ. Cervical radiculopathy: current diagnostic and treatment options. J Surg Orthop Adv. 2009;18(1):13-18.
- Kellgren and Lawrence found that eighty percent of those over age 55 have radiographic changes of degenerative cervical disc disease. (1)
- Lees and Turner found that 45% of patients have one episode of cervical radicular pain and 33% have intermittent attacks. (2)
- Gore and Sepic noted that about a third of their patients had persistent radicular pain and that many of these required surgical treatment. (3)
Clinical Presentation:
- The occurrence of cervical nerve root compression is often insidious without an antecedent injury.
- The pain may be intense, episodic, of long or short duration and may interfere with sleep.
- Avoiding activities which place the neck in extension and lateral bending may lessen symptoms.
- Placing the affected arm behind the head will in most cases relieve tension on the involved nerve roots. (Fig 3)

Fig 3. Relief of nerve root tension by placing arm over the head.
Used with the permission of the Southern Orthopaedic Association. Nasca RJ. Cervical radiculopathy: current diagnostic and treatment options. J Surg Orthop Adv. 2009;18(1):13-18.
- Limited range of motion of the neck is common, especially rotation and lateral bending.
- Radicular pain is increased in the ipsilateral extremity when the examiner places the neck in extension and lateral bending toward the symptomatic side, the Spurling’s test.
- With C5 radiculopathy there is pain to palpation in the suprascapular notch area, weakness of the supraspinatus, infraspinatus and deltoid muscles and numbness to pin prick in the lateral arm over the deltoid.(4)
- With C6 radiculopathy, there is weakness of the biceps, wrist extensors, a diminished biceps reflex and numbness in the dorsal aspect of the thumb and index finger.
- With a C7 radiculopathy there is weakness of the triceps, finger extensors and wrist flexors in association with a depressed triceps reflex and diminished sensation along the dorsal aspect of the long finger.
- With a C8 radiculopathy there is weakness of the intrinsic muscles of the hand and numbness in the ulnar 2 to 3 fingers. (5)
Causes of Cervical Radiculopathy:
- Cervical disc herniation
- Most common cause of cervical nerve root compression.
- Disc usually herniates thru annular fissures in the posterior lateral area of the disc. This will cause pressure on the adjacent root.
- Herniation of the C5-C6 disc will cause a C6 radiculopathy.
- If herniation is directly posterior, may cause compression on the ventral aspect of the dura resulting in spinal cord compression (Myelopathy) as well as nerve root compression.
- On occasion, the nuclear contents will extrude out thru the annular fissures into the epidural space. This may result in “free fragments” of disc material.
- Foraminal stenosis
- Results from the degenerative disc, facet and Luschka joint osteophytes. As disc degenerates, nerve root canals become reduced in size.
- Osteophytes which form along the posterior lateral margins of the disc, Luschka joints and facets may cause irritation or compression on the cervical nerve roots.
- Fractures and dislocations of the cervical spine
- May cause a radiculopathy as well as trauma to the spinal cord.
- Fractures thru the vertebral body involving the posterior lateral corner may cause compression of the adjacent root.
- Bilateral and unilateral jumped facets may result in radiculopathy with or without spinal cord involvement.
- Neurofibromas
- Originate from the connective tissue of neural tissue. As these tumors enlarge they result in intrinsic compression on the nerve root.
- In Neurofibromatosis, multiple nerve roots may be involved with widening of the neural foramens due to the pressure from the enlarging tumors.
- Cervical ribs
- Usually bilateral and may cause compression on the C8 root between the first rib and the aberrant cervical rib.
- Those affected complain of pain and paresthesias in the arm and hand which is often poorly localized to the ulnar side of the hand.
- Compression of the axillary artery and vein may occur with a cervical rib.
- Pancoast tumor
- Malignant tumor of the apical portion of the lung which grows into the lower roots of the cervical brachial plexus.
- Patients present with severe pain in the involved upper extremity with various degrees of neuropathy.
- Syringomyelia
- May present with radiculopathy as well as myelopathy and must be considered as possible etiology.
- Patients with various demyelinating diseases may present with radicular complaints.
Diagnostic Evaluation:
- Needle electromyography is helpful in differentiating nerve compression from nerve root irritation and in confirming the roots involved.
- Can be useful in detecting metabolic and other non-structural causes of radiculopathy.
- Motor and sensory conduction times are performed to evaluate peripheral nerve entrapments which may overlap with cervical neuropathy.
- Electrodiagnostic studies can be useful in following the course of nerve recovery following treatment or injury.
- Considering the prevalence of degenerative changes routine cervical X-Rays may be of limited value in the aging patient.
- Flexion and extension lateral X-rays of the cervical spine are done to assess stability before and after surgery.
- Oblique views may be useful in evaluating facet joint osteophytes and foraminal encroachment.
- Multiplanar reformatted CT scans are helpful in determining the location and extent of the osteophytes responsible for nerve root compression. (Fig. 4.)
Fig. 4. Reformatted multiplanar CT scan showing posterior and foraminal osteophytes at C4-C5.
Used with the permission of the Southern Orthopaedic Association. Nasca RJ. Cervical radiculopathy: current diagnostic and treatment options . J Surg Orthop Adv. 2009;18(1):13-18.
- Cervical myelography with CT may be needed to further clarify the diagnosis in some post-operative patients with persistent or recurrent radicular complaints.
- MRI has been the most useful study in pinpointing the diagnosis and location of the many underlying causes of cervical radiculopathy as well as identifying intrinsic spinal cord diseases, tumors, infections and syrinxes.
- The addition of contrast may be necessary in patients who have had previous surgery and present with recurrent radiculopathy.
Non Operative Treatment:
- Non-operative treatment consists of observation, avoidance of activities which exacerbate the radicular pain and use of NSAIDs.
- Cold applied to tender areas and trigger points may give temporary relief.
- A short course of tapering corticosteroids is effective in decreasing radicular complaints.
- Home cervical traction may be useful as well as motorized traction for short periods of time.
- Avoid neck positions which exacerbate radicular pain like extension when applying longitudinal traction.
- The services of a skilled physical therapist are invaluable in the early management of the patient.
- Manual traction by the physical therapist may be effective.
- Isometric exercises performed by the patient may be helpful.
- Use of a soft cervical collar for short periods, especially when riding in a car.
- Prolonged use of a collar is to be discouraged.
- Selective cervical nerve root blocks under fluoroscopic control may be diagnostic as well as therapeutic.
- Injection of cervical epidural steroids are somewhat controversial and may be associated with significant but rare complications such as meningitis, epidural abscess, epidural hematoma and cord (6) and root injury.
Surgical Options:
- “Key-hole” laminotomy for the treatment of herniated cervical disc was popularized by Scoville (7).
- A small amount of lamina and superior facet is removed to gain access to the epidural space and the underlying compressed nerve root.
- Carefully mobilization of the sensory and motor components of the nerve root and removal of the disc herniation is done.
- Complications include, epidural bleeding, varying degrees of trauma to the nerve root due to manipulation and recurrent herniation.
- If done in the sitting position air embolism may occur but this complication is infrequent.
- Anterior approaches to the cervical spine for treatment of degenerative disc disease and herniated disc were reported by Smith and Robinson at Johns Hopkins in 1958 (8).
- Some surgeons performed anterior discectomies without fusion, but this procedure resulted in kyphotic deformity and instability in some patients necessitating further treatment.
- The procedure of anterior disc removal and interbody fusion (ACDF) with autogenous bone graft has become the gold standard of treatment.
- Smith and Robinson reported good clinical, functional and radiographic results from their procedure.
- They also noted resolution of osteophytes at the operative level(s) in patients who achieved a solid interbody arthrodeses.
- Because of this observation, they did not recommend removal of osteophytes during the index operation.
- Shen, et al. (9) did a comparative study on outcomes of anterior cervical discectomy and fusion with anterior plate fixation with and without direct uncovertebral joint decompression and found no difference in the clinical and radiographic results.
- Critical to the success of the operation is precise localization of the involved levels(s), removal of free fragments of disc behind the posterior longitudinal ligament, proper preparation of the vertebral endplates, and sizing and insertion of the bone graft under compression.
- Wang, et al. found that anterior cervical plates have added to the stability of multiple level grafts without adding a great deal of time to the procedure (10).
- Intra-operative SSEP and MEP monitoring has contributed to the safety and reduction in neural and spinal cord complications.
- Spinal cord and nerve root damage may occur but are rare.
- Nonunion of the arthrodeses occurs in a small number of patients.
- The use of anterior plates has reduced the rate of failed fusions and graft displacement.
- Degeneration of disc segments adjacent to the fused levels may occur following successful surgery (11).
- There is some evidence that this may be the result of increased mechanical forces on these adjacent discs, failure to recognize symptomatic adjacent levels at the time of the index operation or the result further progression of degenerative disc disease.
- Cervical microendoscopic discectomy and foraminotomy done thru a small posterior incision has gained popularity for treating unilateral radiculopathy due to disc herniation and cervical foraminal stenosis.
- The procedure is not to be done in cases of cervical myelopathy.
- Advantages include short operative time, same day surgery, and early return to work with few complications.
- Adamson noted few complications, resolution of neuropathy and good to excellent results in the 97 of 100 patients. (12)
- Anterior cervical microforaminotomy has been described by Hae-Dong Jho (13).
- This procedure is done thru an open anterior-lateral approach or by an endoscopic technique.
- In a series of 104 patients Jho reported only one fair result. (13)
- Complications included 2 transient Horner’s syndromes which resolved in 6 weeks and a discitis that went on to spontaneous interbody fusion.
- The early results of cervical disc replacement (CDR) are promising. (14)
- Several cervical disc replacement implants are in clinical trials.
- The advantages of disc replacement over fusion are reported to be less loss of motion and possibly less chance of adjacent segment degeneration.
- Rhee, et al. noted the possibility of osteophytes reoccurring following cervical arthroplasty rather than their resolution as seen following successful fusion. (4)
Complications:
- Dysphagia and hoarseness due to recurrent laryngeal nerve compression are the most common post-operative problems following ACDF.
- The incidence calculated from the literature by Baron, et al. is 12.3% for dysphagia and 4.9% for hoarseness. (15)
- Most cases of post-operative hoarseness and difficulty swallowing are of short duration.
- Vocal cord paralysis is rare.
- Perforations of the esophagus and trachea are rare.
- Proper positioning of retractor blades and frequent release of tension on the soft tissue will decrease the incidence of these complications.
- Apfelbaum, et al. have related the cause of recurrent laryngeal nerve palsies to the pressure of the endotracheal tube against the nerve within the endolarynx (16). Deflating and reinflating the endotracheal cuff reduced transient vocal cord palsies from 6.8% to 1.7%.
- Vertebral artery injuries are rare as are spinal cord injuries. Kraus and Stauffer reported a 0.3 % incidence of spinal cord damage. (17)
- C5 radiculopathy may occur after both anterior and posterior approaches to the cervical spine (18).
- It may be immediate or delayed. Direct nerve root injury is rare.
- Extrusion of bone grafts and nonunion occurred in uninstrumented anterior cervical fusions.
- The addition of anterior cervical plates has resulted in higher rates of fusion and has eliminated graft extrusion.
- Rigid anterior plate instrumentation has been reported by Samartzis, et al. to result in allograft fusion rates equal to those of autografts. (19)
- Screw and plate breakage is rare.
Post-operative Care
- Drains are rarely necessary.
- X-rays prior to closure to be sure that the proper levels have been treated and that the bone graft(s) and instrumentation have been correctly placed. (20)
- A cervical collar is optional.
- Antibiotics are continued for 24 hours.
- Short course of post-op steroids is often used to decrease airway edema.
- Diet will depend on the degree of swallowing difficulty the patient experiences.
- Solid and dry foods are best avoided in the early post-operative period.
- Radiographs are done at 6 and 12 weeks to monitor the healing of the bone graft(s).
- Collars are removed while awake but recommended while traveling in a car until X-rays show signs of bone graft healing.
Conclusions:
- A precise diagnosis is imperative before embarking on a treatment for cervical radiculopathy.
- About a third of patients with persistent cervical radiculopathy may need surgical treatment.
- ACDF is a well proven surgical procedure.
- Total Cervical Disc Replacement is promising.
References:
- Kellgren J, Lawrence J. Osteo-arthrosis and disc degeneration in an urban population. Ann Rheum Dis. 1958;17(4):388-397.
- Lees F, Turner J. Natural history and prognosis of cervical spondylosis. Br Med J. 1963;2(5373):1607-1610.
- Gore D, Sepic S. Anterior cervical fusion for degenerative or protruded disc. Spine 1984;9(7):667-671.
- Levine MJ, Albert TJ, Smith MD. Cervical radiculopathy: Diagnosis and nonoperative management. J Am Acad Orthop Surg. 1996;4(6):305-316.
- Rhee JM, Yoon T, Riew KD. Cervical r adiculopathy. J Am Acad Orthop Surg. 2007;15:486-494.
- Hodges SD, Castelberg RL, Miller T, et al. Cervical epidural steroid injection with intrinsic spinal cord damage. Two case reports. Spine 1988;23:2137-2142.
- Scoville WB. Types of cervical disc lesions and their surgical approaches. JAMA 1966;196(6):479-481.
- Smith GW, Robinson RA. Treatment of certain cervical spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40A:607-624.
- Shen FH, Samartzis D, Khanna N, et al. Comparison of clinical and radiographic outcome in instrumented anterior cervical discectomy and fusion with and without direct uncovertebral joint decompression. Spine J. 2004;4:629-635.
- Wang JC, McDonough PW, Kanim LE, et al. Increased fusion rates with cervical plating for three level anterior cervical discectomy and fusion. Spine 2001;26:643-647.
- Ishihara H, Kanamori M, Kawaguchi Y, et al. Adjacent segment disease after anterior interbody fusion. Spine J. 2004;4(6):624-628.
- Adamson TE. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy. J Neurosurg. 2001;95(1 suppl):51-57.
- Jho HD. Microsurgical anterior cervical foraminotomy for radiculopathy: a new approach to cervical disc herniation. J Neurosurg. 1996;84(2):155-160.
- Watts J, Guyer RD. Cervical Total Disc Replacement, “Wheeless Textbook of Orthopaedics,” wheelessonline.com. Published April 21, 2016.
- Baron EM, Soliman AM, Gaugham JP, et al. Dysphagia, hoarseness and unilateral true vocal fold motion impairment following anterior cervical discectomy and fusion. Ann Otol Rhinol Laryngol 2003;112(11): 921-926.
- Apfelbaum RI, Kriskovich MD, Haller JR. On the incidence, cause and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine 2000;25(22):2906-2912.
- Kraus DR, Stauffer ES. Spinal cord injury as a complication of elective anterior cervical fusion. Clin Orthop Relat Res. 1975;(112):130-141.
- Tsuzuki N, Zhogshi L, Abe R, et al. Paralysis of the arm after posterior decompression of the cervical spinal cord. I. Anatomical investigation of the mechanism of paralysis. Eur Spine J. 1993;2(4):191-196.
- Samartzis D, Shen FH, Matthews DK, et al. Comparison of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine J. 2003;3(6):451-459.
- Nasca RJ. Cervical radiculopathy: current diagnostic and treatment options . J Surg Orthop Adv. 2009;18(1):13-18.
- See:
- Brachial Plexus - Neuro Exam
- Diff Dx of Cervical Pathology
- Neuro Exam
- PE of the C-spine
- PE of Lumbar Spine
Discussion:
- can be associated with myelopathy;
- can involve one or multiple roots, and symptoms include neck, shoulder, and arm pain, paresthesias, and numbness;
- findings may overlap because of intraneural intersegmental connections of sensory nerve roots;
- lower nerve root at a given level is usually affected;
» Examination of the Cervical Spine:
Spurling's Manuever:
- mechanical stress, such as excessive vertebral motion, may exacerbate symptoms;
- the provocation of the patient's arm pain with induced narrowing of the neuroforamen
- gentle neck hyperextension with the head tilted toward the affected side will narrow the size of the neuroforamin and may exacerbate the symptoms or produce radiculopathy;
- ipsilateral rotation of the neck will also increase radiculopathy;
- downward head compression increases the patient's radicular pain and paresthesias, especially if the neck is flexed to the side of involvment;
Shoulder Abduction Relief Test:
- significant relief of arm pain with shoulder abduction;
- this sign is more likely to be present w/ soft disc herniation, whereas, the test is likely to be negative with radiculopathy caused by spondylosis (osteophyte compression);
Tinel's Sign:
- in radiculopathy, direct palpation or percussion over the exiting nerve root may provoke the patient's familiar limb or axial pain;
- if the tenderness or a Tinel's sign is elicited more laterally, such as in the supraclavicular fossa, then the diagnosis should be questioned;
Surgical Treatment: (see spondylosis)
- in the study by Sampath P, et al (1999), while 75% of patients had a satisfactory outcome, 25% continued to have persistent excruciating or horrible pain

