- See:
- See:
- operative considerations for hip dyplasia
- reaming technique:
- component insertion:
- component position:
- screw placement:
- acetabular component revision:
- bone grafting for acetabular defects:
- Discussion:
- U shaped portion of acetabulum (fovea) w/ articular cartilage normally protrudes above the true floor
(quadralateral plate) of acetabulum by a few milimeters;
- floor of acetabulum corresponds to lateral aspect of radiographic teardrop;
- fovea / true floor of pelvis:
- identification of the true floor is essential for determining depth of acetabular reaming;
- reaming to depth that obliterates the fovea (U shaped portion of acetabulum) usually converts bony acetabulum to
hemisphere;
- one should rarely ream deeper than true floor of acetabulum;
- moving the hip center medially improves the efficiency of the hip abductors and will reduce the forces acting on the hip in the
coronal plane;
- reference: The Acetabular Fossa May Not Be Located at True Center of Acetabulum: A Detailed Analysis Using Preop CT
- considerations in rheumatoid arthritis:
- acetabular erosion may result in protrusio (medial and proximal hip migration);
- in this case the hip center must be re-established laterally and inferiorly;
- considerations in osteoarthritis:
- acetabulum is often overgrown by osteophytes that push the femoral head laterally, superiorly, and posteriorly;
- in order to re-establish optimal hip mechanics, the hip center must be placed medially, inferiorly, and anteriorly;
- note that medialization down to the true inner table which decreases the offset more than 1 cm will weaken the abductors, will
increase joint reaction forces, and may lead to THR instability;
- this decrease in offset can be managed appropriately by using an increased offset femoral stem;
- Radiographs:
- radiographic teardrop:
- true floor of acetabulum corresponds to the radiographic teardrop;
- teardrop lies in the inferomedial portion of the acetabulum, just above the obturator foramen;
- lateral and medial lips corresponds to the external and internal acetabular walls, respectively;
- medial wall is a relatively constant radiographic finding and is not significantly distorted by small degress of rotation (unlike
ilioischial line - Kohler's line);
- the tear drop gives an accurate assessment of how much medialization is necessary to have the acetabular component rest
on the true acetabular floor;
- tear drop may appear less prominent on obturator oblique views;
- ilioischial line: (Kohler's line)
- as pointed out by Goodman, et al (1988), the ilioischial line does not consistently represent the true acetabular floor;
- anatomically the superior ilioischial line is formed by the broad cortical surface of the siciatic notch (which lies posterior to
acetabular floor), and the inferior ilioischial line is formed by the cortical surface of the anteiror ischium;
- hence, anatomically this line does not correspond to the acetabular floor;
- on straight AP radiographs, the ilioischial line will overlie the acetabular floor, but with any amount of rotation, this
relationship will diverge;
- indeed, the entire medial wall may be reamed out, without disrupting Kohler's line;
- references:
- The acetabular tear drop and its relevance to acetabular migration.
- Technique:
- remove ligamentum teres & w/ curet remove the cartilage and soft tissue from the acetabulum;
- use true floor of acetabulum as marker for the depth of reaming;
- one should rarely ream deeper than true floor of acetabulum;
- if osteophytes have grown over the true acetabular floor (forming a unicortical plate), break thru these w/ w/ a gouge, osteotome,
or small reamer to expose the soft tissue components of the acetabular floor;
- in this case, central portion of the bony acetabulum requires more reaming than the periphery;
- typically an 1/2 inch osteotome is used to chisel the outline of the old fovea and then the osteotome is used to chisel a cross
across the floor of fovea;
- usually the osteotome will break through the brittle osteophytic bone, but it will usually not disrupt the underlying inner
table (except in patients w/ osteoporosis);
- after a cross has been chiseled into fovea, osteotome is used to pry out osteophytes (diseased bone will usually pry out
where as inner table will not);
- after removal of tissue from acetabular fossa, true floor of acetabulum is exposed;
- by measuring the depth of this trough, the surgeon can also accurately ascertain the depth of reaming;
- avoid excessive medialization:
- it is important to establish the level of the inner table in the superior half of the fovea;
- if the surgeon attempts to locate the inner table in the lower half of the fovea (near the obturator foramen), there is a
possibility of over-medialization (since the acetabulum slopes in a supero-lateral to a infero-medial direction;
- furthermore, using the lower portion of the fovea as a reference point, risks placing the cup in an excessively
inferior position;


- avoid excessive lateralization:
- failure to ream upto the true acetabular floor will have three negative effects;
- lateralization of the acetabular cup (increasing joint reactive forces);
- uncoverage of the superior acetabular cup (or inappropriate abduction of of the cup to achieve coverage);
- positioning of the cup in an area of suboptimal vascularity;
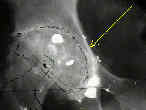
- Case Example:
- 35-year-old male w/ near anklyosed hip following a GSW to the hip;
- preoperative films appeared to indicate that little or no medialization was necessary, but a careful look shows that the film is
slightly rotated;;
- postoperative films, however, indicate that the cup was lateralized (hence, reaming was inadequate)
Secondary total hip replacement after fractures of the femoral neck.
Current status of acetabular fixation in primary total hip arthroplasty.
Benefit of cup medialization in total hip arthroplasty is associated with femoral anatomy